How exact RUG minutes under Medicare Part A can hurt your SNF…
On March 9, 2016, CMS announced the release of new “SNF Utilization and Payment Data.” This payment information includes Medicare Part A services provided by skilled nursing facilities nationwide. This SNF PUF, or Skilled Nursing Facility Payment Public Use File, contains information including therapy and nursing utilization, RUG scores and payments for over 15,000 SNF’s totaling $27 billion in Medicare payments for one year – 2013.
*Update: CMS has now posted data for CY2014 – click here to view and download tables.
Upon releasing this data, CMS stated:
“The Skilled Nursing Facility data released is yet another example of our commitment to greater data transparency. CMS believes that when information flows more freely, the health care system functions more efficiently. This leads to better care, smarter spending, and healthier people.”
Why Is This Data Release Important to SNF Professionals?
It is NOT news to anyone that CMS has focused in on over-utilization of the Rehab Ultra RUG – and this data file has usage information for all SNF’s. What IS news, however, is what CMS said they will now be looking at in more detail – total therapy minutes.
The SNF PUF data has confirmed information that has been consistent with prior CMS findings with Ultra-High (RU) and Very High (RV) Rehabilitation RUGs. The SNF PUF shows that for these two RUGs, the amount of therapy provided is often very close to the minimum amount of minutes needed to qualify a patient for these categories. {Meaning – the bare minimum is being provided to hit the RUG}
The PUF data showed:
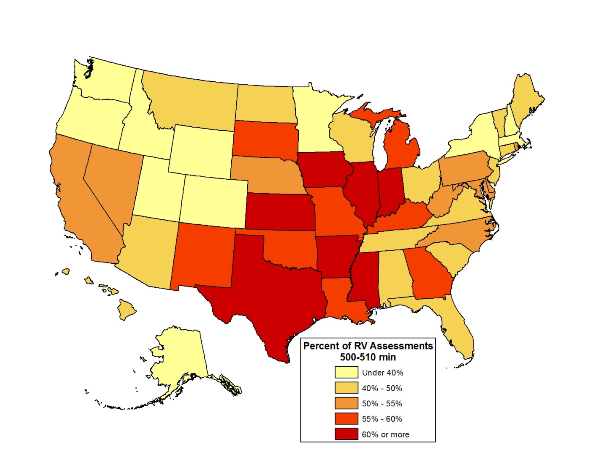
- 51 % of all RV scores = Therapy provided between 500-510 minutes.
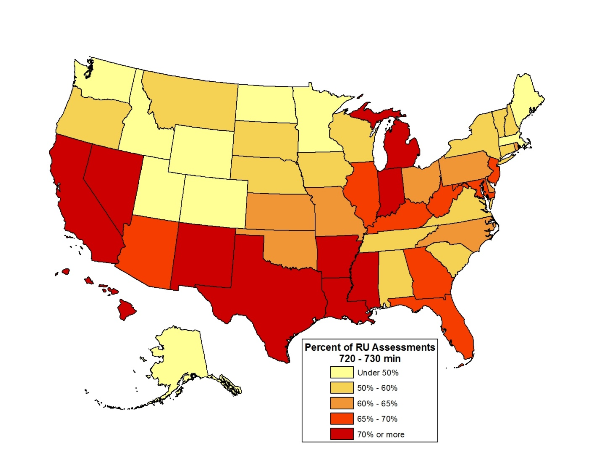
- 65 % of all RU scores = Therapy provided between 720-730 minutes.
- For 88 providers, all of their RV scores =Therapy provided between 500-510 minutes.
- For 215 providers, all of their RU scores =Therapy provided between 720-730 minutes.
- More than one in five providers had more than 75 percent of both RU and RV scores =Therapy provided within 10 minutes of the minimum threshold.
How did your state perform? (Remember, this is 2013)
Why Is This Happening and Why Is It “Bad?”
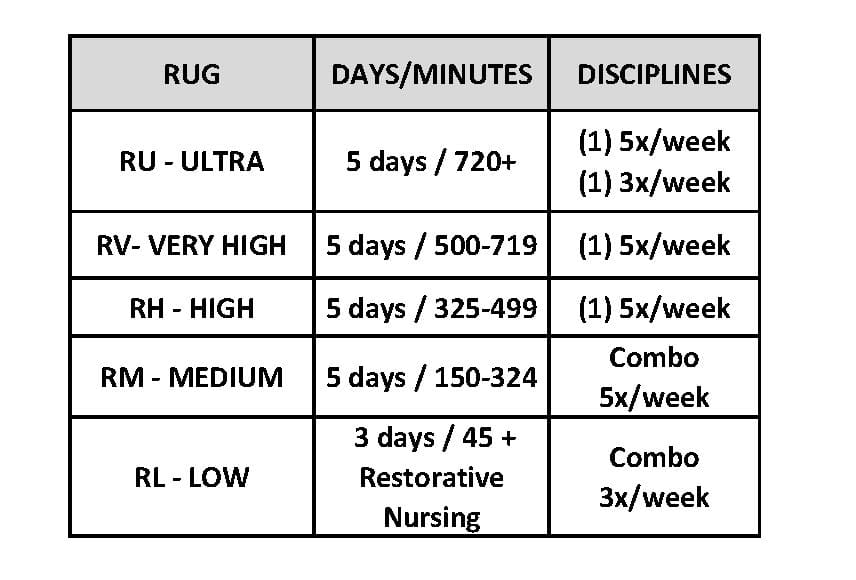
As you know, therapy RUG scores are based on the total number of minutes provided in the 7 day assessment window. Each RUG category has a range of minutes with a bottom and ceiling. Just one minute over the ceiling will get you into the next RUG category. For a more detailed review of RUGs, read this.
When the SNF PPS Final Rule was published in 1999, specifics of the RUG system development were detailed, including the intent of the breakdown and therapy minute expectations. [Federal Register / Volume 64, No. 146 / Friday, July 30, 1999 / Rules and Regulations ]
The Final Rule stated: “The minutes used to classify beneficiaries into RUG–III groups are in no way to be taken as upper limits. The 720-minute threshold for the Ultra High sub-category is a minimum for purposes of classifying residents. In fact, during the demonstration project, there were beneficiaries who were receiving more than 1,000 minutes per week, and we expect that there will be similar instances during the national implementation. All of the groups were created based on a continuum of minutes being provided, including Ultra High. Just as we expect to see beneficiaries in the High Rehabilitation sub-category receiving 450 minutes per week, we expect that as many minutes as are needed will be provided to beneficiaries in the Ultra High groups.” (Federal Register 7/30/99 -Page 41663 – Top left paragraph)
This rule has never changed – though over the years since its’ implementation, the method in which therapy services are delivered in the SNF setting has – at least in enough SNF’s to call this a “problem.”
As the PUF data indicated, in many cases, therapy is being provided at the “bare minimum” of the RUG category, often exactly on the threshold. How? Many therapy providers schedule pre-planned therapy sessions with the total minutes of the 7 day assessment window hitting the RUG minimum exactly. Often minutes are adjusted daily to hit the “magic number” needed. Why? Minutes are planned out to ensure the targeted RUG is captured. Any “extra minutes” above the minimum number needed to achieve the RUG may be seen as “wasted minutes.” {Cringe} This “overage” cuts into the number of widgets a therapist can produce number of patients a therapist can treat without detracting from the profit margin. Ask any Rehab Manager about “productivity” and “overages.” {Be prepared to duck.}
This “exact science,” or therapy-to-the-minute, may be a red flag that therapy is not necessarily being provided according to resident “need.” How can it be? It would be a pretty big coincidence if in a 7 day window, a majority of residents happended to receive 720 minutes exactly of “reasonable and necessary” therapy, not a minute more or minute less. When therapy is provided based on actual “need,” #1, sessions can’t be scheduled out to the minute, and #2, session length can’t be the same for everyone. Sure, you can have a schedule, but is should be more of a guide and not a rule-book. Remember, Medicare only pays for therapy that meets the guidelines of skilled, reasonable and necessary. The burden is on the SNF to prove this!
Rehab software has also contributed to the problem. Rehab software was designed to assist a therapy manager in scheduling and tracking therapy minutes and RUGs. It was never designed to limit therapy provision down to the minute, though some therapy managers are being asked by management to schedule to the RUG threshold. Therapy managers that are “new” to the SNF world may not even realize what the Federal Register says – and may view the software as their guide as to what Medicare will or will not allow. {Bigger cringe}
What Is CMS Doing About It?
With the release of the SNF PUF data, Dr. Shantanu Agrawal, Deputy Administrator for Program Integrity and Director of the Center for Program Integrity, stated:
“CMS strives to ensure that patient need, rather than payment system incentives, are driving the provision of therapy services. These concerns have prompted us to refer this issue to the Recovery Auditor Contractors (RAC) for further investigation, and our hope is that data transparency will facilitate real changes.”
Recovery Auditor Contractors do just that…audit and recover Medicare $$$ from the SNF.
This statement sounds an awful lot like the DOJ statements surrounding the multiple SNF False Claims Act lawsuits and Settlement Agreements. Remember this one ?
“When seeking payment for federal healthcare programs, it is the providers obligation {the SNF} to assure that services provided to beneficiaries are supported by evidence {documentation} that the services are reasonable and necessary. The DOJ is committed to ensuring that healthcare providers who provide medically unnecessary services to Medicare beneficiaries solely to increase their own profits will be held accountable.”
What Can You Do?
If you haven’t already, it is time to take a good, hard look at both your therapy scheduling practices and documentation.
Gone are the days when a billing log with therapy minute totals and a quick note were enough to support the Rehab RUG. Now it is the therapy documentation behind those minutes that justifies the service and proves the “necessity” which supports the RUG. Therapy documentation must support the RUG billed on the claim, or the SNF risks recoupment of those Medicare dollars. If your facility is one with a high % of RUGs in the RU or RV category, and if your therapy minutes fall on the threshold of the RUG, it is imperative that a reviewer can conclude from the documentation, why this is happening and that the services were reasonable and necessary.
If you are using therapy software to schedule out treatments, the length or intensity of those treatments should be able to be traced back to the therapy evaluation and/or supporting documentation. If it does not, how will you ever differentiate why 1 total hip replacement required a RU level of therapy and another required RH? {And please don’t say the minutes provided are based on type of insurance!} If you schedule out your therapy for a consistent number of minutes per day and allow the exact session length to be determined by the treating therapist, you may have a much easier time proving reasonable and necessary than if you adjust treatment minutes daily based on what is needed to hit the RUG exactly on each assessment reference date. How can you justify saying a resident needs 10 less minutes tomorrow because they received 10 extra minutes today? That mentality is not “need-based.”
In addition to looking at how you schedule your therapy minutes, at a minimum, therapy documentation should also:
- Ensure the therapy plan is developed based on resident need
- Therapy RUGs cannot be set or directed by management and/or financial targets
- Reflect individualization
- Do all your therapy treatment plans look the same? A treatment plan is an individualized plan that should describe what the resident needs, how much the resident needs, and why the resident needs it
- Support the amount of therapy needed from the initial evaluation through to the discharge summary
- Include notes to justify any “ups and downs” in RUGs along the way (especially ups!)
- Show why your residents are receiving therapy at the current RUG level
- Medicare wants to know why. There should be a clinical reason for the difference in minutes provided. Medicare needs to be able to find the answer to that question in your documentation
Don’t be afraid to discuss the RUG category the resident is in and why. How can you justify the RUG if you never mention it? An interdisciplinary team (IDT) note for each completed MDS that states the “achieved RUG” and why it is indicated for a particular resident would be a great start in providing a reviewer with concrete information about the circumstances of the therapy service intensity. It is up to each facility to prove to a Medicare reviewer that the resources utilized to achieve the RUG scores billed were “reasonable and necessary.”
We know first hand how valuable therapy services are to the SNF population. Take a few extra minutes to document your value! Show Medicare. The last thing any provider wants is for CMS to audit and pull the RUG out from under them.
In your corner,
Dolores
www.MonteroTherapyServices.com Providing Training, Education and Support to SNF’s Nationwide
IMPORTANT LINKS:
To view the 3/9/16 CMS Press Release on SNF PUF data, click here.
To view the Fact Sheet on the Skilled Nursing Facility PUF data set, click here.
To view the Medicare Provider Utilization and Payment Data for SNF Home Page, as well as all data, click here. {You can now view 2103 and 2014 data}
Is your SNF “on the list?” **To see how your SNF did – view the Medicare Therapy Minutes Aggregate Table, CY 2014, Microsoft Excel (.xlsx)