With each passing year, the amount of information SNF therapy and MDS professionals need to digest grows and grows, and it can be overwhelming. This comprehensive summary is intended to be an instructional guide for SNF therapy and MDS professionals.
Print this, punch some holes in it, put it in a binder, and keep it as a resource to help you through the next year.
Take each of the 3 main pieces 1 bite at a time.
1- Part A Rate, PDPM, and MDS Changes
2- SNF Quality Reporting Program (SNF QRP)
3- SNF Value Based Purchasing (SNF VBP)
Centers for Medicare and Medicaid Services (CMS) released the Medicare Part A Skilled Nursing Facility (SNF) Prospective Payment System (PPS) FY2025 Final Rule containing the components that will go into effect 10/1/24. The Final Rule provides updates to Part A rates, ICD-10 Code mapping for Patient Driven Payment Model (PDPM) calculations, SNF Quality Reporting Program (SNF QRP) changes, and SNF Value Based Purchasing (SNF VBP) updates.
Taking time to understand where the information comes from and what it means will help you help your facility succeed.
Medicare Part A Rate & PDPM Changes
Medicare Part A Rates
The Federal Per Diem rates are updated annually. On 10/1/24, the rates for Part A will have a net increase of 4.2%, which means an increase of $1.4 billion in Medicare Part A payments to SNFs in FY2025. That may sound like a lot, but to put this in perspective, if all 15,000+ SNFs received equal shares, this would equate to [only] $93,000 more per SNF, and that’s before the deductions from the SNF QRP and VBP are factored in.
The details of how 4.2% is derived can be found below.
- [(SNF Market Basket increase of 3.0% + Forecast Error Correction of 1.7%) – 0.5% Productivity Adjustment (MFP)] = 4.2%.
- CMS updated one of these variables this year. The SNF Market Basket base year was updated to use info from 2022, instead of 2018. This type of update was last done 3 years ago when the base year was updated from 2014 to 2018…. so change, in this case, is good!
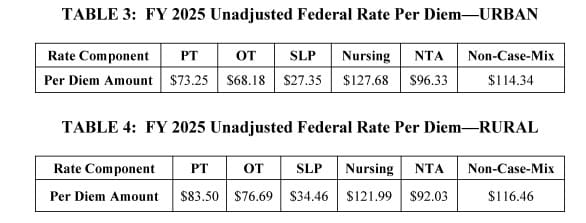
Below are the final “Unadjusted” Federal Per Diem rates for 10/1/24. These rates are important variables as they are used to calculate each Patient Driven Payment Model (PDPM) Case Mix Group (CMG) rate. They are “unadjusted” because they have not yet been multiplied by a Case Mix Index value.
Once we have the daily per diem rate information above, we can put this together with changes to the Case Mix Index values in the next section to outline the individual rate for each Case Mix Group. This will make the “unadjusted” rates “adjusted” for each Case Mix Group. More on that below.
Medicare Part A PDPM Changes – Case Mix Index Values
Case Mix Index (CMI) values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, are updated annually as needed. These values are important as they assign “weight” to each of the CMGs, and when multiplied by the daily per diem rates in the prior section, determine the rate for each individual CMG.
For the last 2 years, CMS reduced these CMI values as a means to solve the problem of having SNFs “pay back CMS for overpayments” related to the “PDPM Recalibration.” CMS adjusted the CMI values to produce an overall lower Medicare Part A daily payment rate. Thankfully, we are over the recalibration hurdle now, and the CMI values for each of the 5 components for 10/1/24 will be the same as last year. The dollar values will be different, of course, due to the 4.2% rate change, but the CMI values will remain the same.
Here are the final “adjusted” daily rates for each of the case mix groups (CMG), derived by multiplying the Unadjusted Federal Per Diem Rate with the CMI value assigned to each CMG. These are the pieces needed in order to calculate the total daily rate.
Total Daily Rate = PT + OT + SLP + Nursing + NTA + Non-Case Mix Rate (Flat Rate)
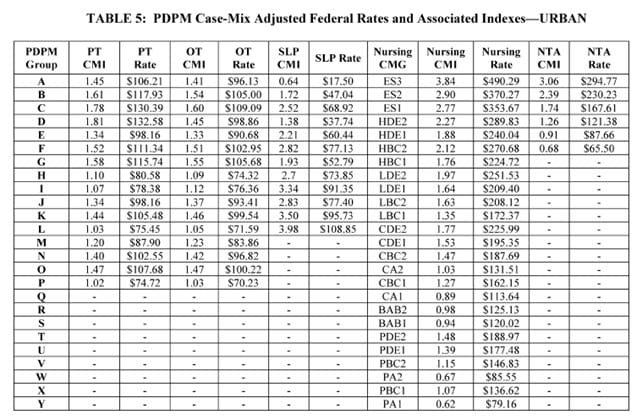
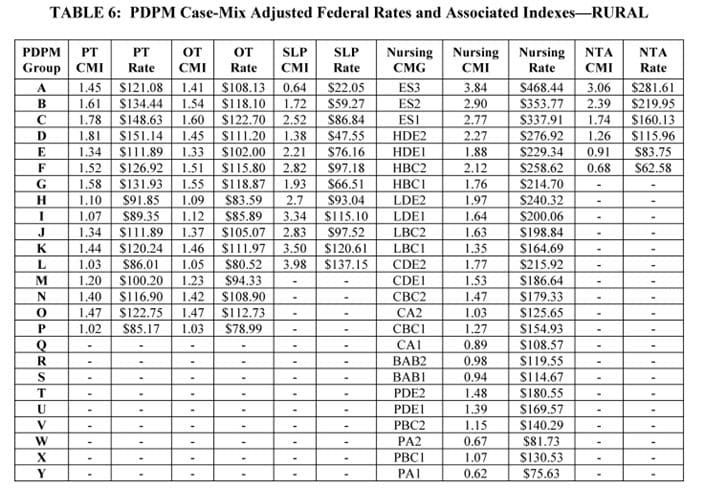
As a reminder, all of the CMG scores come from the MDS and how trigger questions are answered. The Non-Case Mix Group Rate is a “flat rate,” not tied to the MDS.
For example, using the chart above, a HIPPS Code of KACD1 represents TK [PT $105.48] + TK [OT $99.54] + SA [SLP $17.50] + ES1 [Nursing $353.67] + ND [NTA$121.38] + Non-Case Mix Rate [$114.34]. The total base rate for this HIPPS Code would be $811.91 per day.
The total base rate per day fluctuates based on what “PPS day” it is. Days 1-3 see a higher rate due to the NTA Component paying triple, and days 21-100 see a rate reduction as the PT and OT Component slowly decreases in value throughout the stay.
With the above charts, you can calculate the general daily per diem rate for any HIPPS code. To calculate the rate unique to your SNF, you will need the Wage Index information in the next section.
Changes In Wage Index – Geographical Locations – For part a rate calculation
In the section above, we demonstrated how to calculate the daily per diem rate. To take this rate and transform it into the rate that your SNF will receive, requires another piece of the puzzle…. the Wage Index (WI).
CMS categorizes SNFs as Urban or Rural and assigns a unique WI value to each county or state. This WI is a variable used to take the Total Daily Per Diem Rate and adjust it up or down based on where you live.
The total daily rate explained in the section above is comprised of a Labor Portion and a Non-Labor Portion. The WI is used to adjust the Labor Portion to get your location-specific rate, as different parts of the country are reimbursed at different rates.
Total Daily Rate = Labor Portion + Non-Labor Portion
Your SNFs Total Daily Rate = (Labor Portion x Your SNFs Wage Index) + Non-Labor Portion
CMS updates these WI values each year. The Final Wage Index Tables for FY 2025 can be found here:
The Final Rule made some changes to Urban and Rural classifications, flipping 54 counties from Urban to Rural, and 54 from Rural to Urban. The Rule also changed the way some of the counties are grouped together, impacting the overall rate for many. To view all the specific county changes, see page 38 of 116 in the Final Rule PDF.
You should know whether your SNF is Urban or Rural, as well as your area WI. Not sure of either? Use the Wage Index Look Up Tool HERE and plug that into the PDPM Calculator to get your rates.
Medicare Part A PDPM Changes: ICD-10 Code Mapping For PT, OT & Speech Components
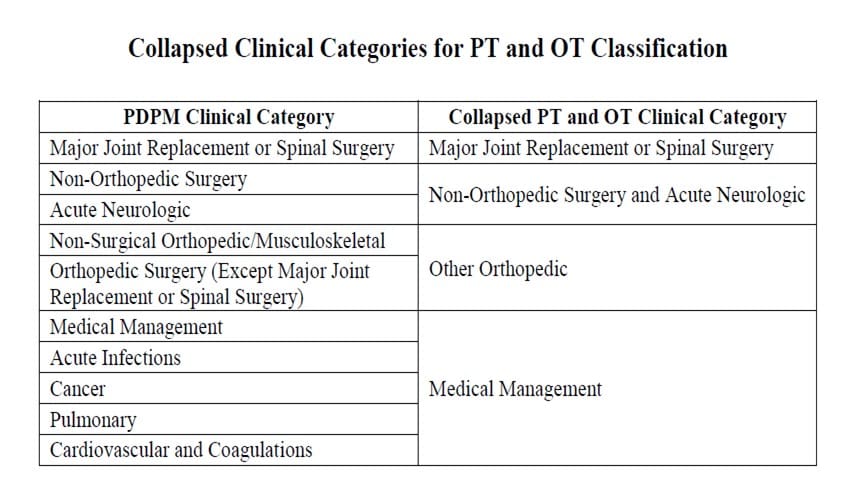
The ICD-10 Code selected for MDS Section I0020B as the primary reason for SNF Part A covered care is used for case mix classification under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, and if not mapped to one of these, it is then deemed a “return to provider” code.
In other words, Return to Provider Codes can’t be used to represent the primary reason for skilled care in Section I0020B, and the code that is used in this Section will fall into 1 of the 4 collapsed Clinical Categories below, thus, determining the PT/OT Component grouping, and the 1st letter of the HIPPS code, or “MDS Score.”
Each year, CMS makes modifications to the mapping of certain ICD-10 Codes. Believe it or not, there are only 4 code changes for FY2025, changing the mapping from Medical Management to Return to Provider.
These 4 codes are:
- E88.10 Metabolic Syndrome
- E88.811 Insulin Resistance Syndrome, Type A
- E88.818 Other Insulin Resistance
- E88.819 Insulin Resistance, Unspecified
Here is the new CMS Mapping file which includes all the code changes for 10/1/24:
FY 2025 PDPM ICD-10 Mapping (ZIP)
Future Changes to the Non-Therapy Ancillary (NTA) Component
CMS received multiple comments from the Proposed Rule “Request for Information (RFI)” regarding a future restructuring of the NTA component. Though NTA changes are not happening for 10/1/24, CMS states the NTA Component will change, and they are taking into account the comments and feedback received by providers after the Proposed Rule was issued.
The Rule outlined in great detail what the NTA changes would look like, if/when they occur. The reason for the makeover is due to updated NTA and Part A PDPM claims data from FY2019-2022.
Proposed future updates include modifying where the NTA points “come from.” We know that points can come either from checkboxes on the MDS or by adding ICD-10 Codes to Section I8000 from the Mapping Files, and there can often be confusion, as some point categories are listed in both places, but the points can only come from one source. CMS intends to rely more on MDS checkboxes when possible.
A NTA Component simplification process for coding will be welcomed! Our chart reviews often identify missed NTA point opportunity simply based on the inconsistencies of the component. Here are a few current examples that illustrate why clarification in the NTA Component would be welcomed:
- Checking Cirrhosis in Section I1100 will not capture 1 NTA point. The ICD-10 code from the CMS Mapping File under the Cirrhosis category must be entered into Section I8000 for the point.
- Checking Respiratory Failure in Section I6300 will not capture 1 NTA point. The corresponding ICD-10 Code from the CMS Mapping File under Cardio-Respiratory Failure and Shock is required to gain the point.
Eliminating the duplication will improve accurate coding and reimbursement.
Potential Changes to the NTA Component Point Value
The changes under consideration to the NTA Component are shown below. This is what the “new NTA Point List” would look like if all changes were made.
Points highlighted in red reflect a reduction from the current point value, and green, an increase in point value.
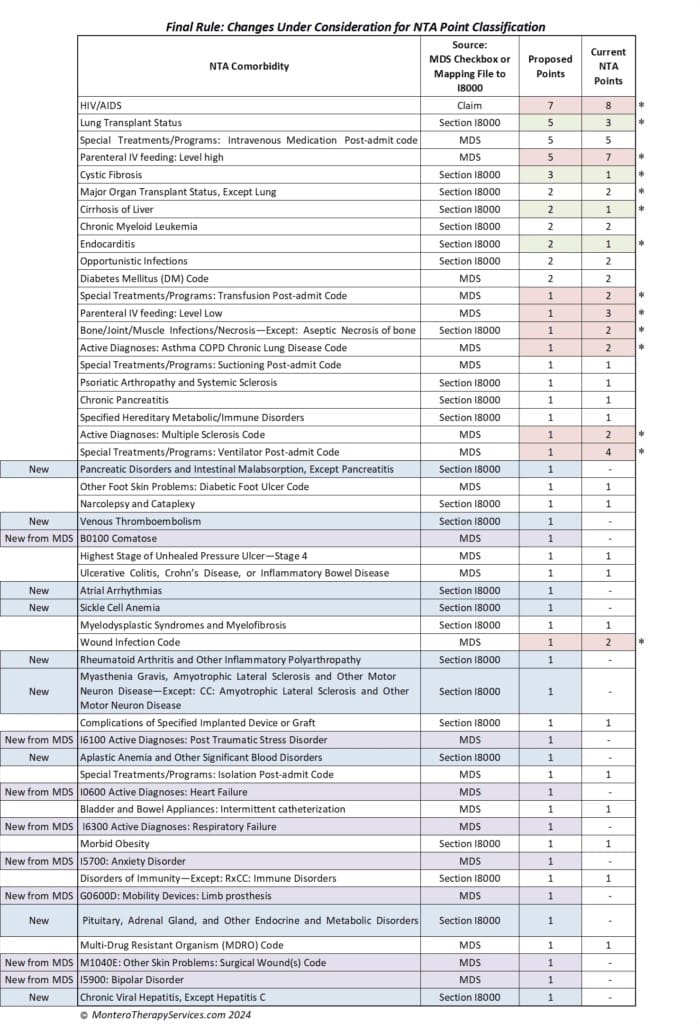
9 Items Dropping in point value are: HIV/AIDS, IV Feeding: High and Low Level, Transfusion Post Admit, Bone/Joint/Muscle Infections, I6200 Asthma/COPD, Ventilator Post Admit, Multiple Sclerosis, and Wound Infection.
4 Items Gaining point value are: Lung Transplant Status, Cystic Fibrosis, Cirrhosis, and Endocarditis.
The blue and purple areas represent the additions to the NTA point family. These include MDS checkbox items and Section I8000 add-ons. It is interesting to see some of these checkbox additions:
- Section B: Comatose
- Section G: Limb Prosthesis
- Section I: PTSD, Heart Failure, Respiratory Failure, Anxiety Disorder, and Bipolar Disorder
- Section M: Surgical Wounds
NTA Point Categories Removed From The List
Last but not least, let’s look at NTA points that would be eliminated. Though the categories for removal only have 1 point value, we know that only 1 point is needed to move from NF to NE… a big difference in reimbursement… over $20 per day!
There are some frequent flyers here that will make a big difference in facility comorbidity scores if removed. It’s not a shocker to see Malnutrition, among others, on the list.
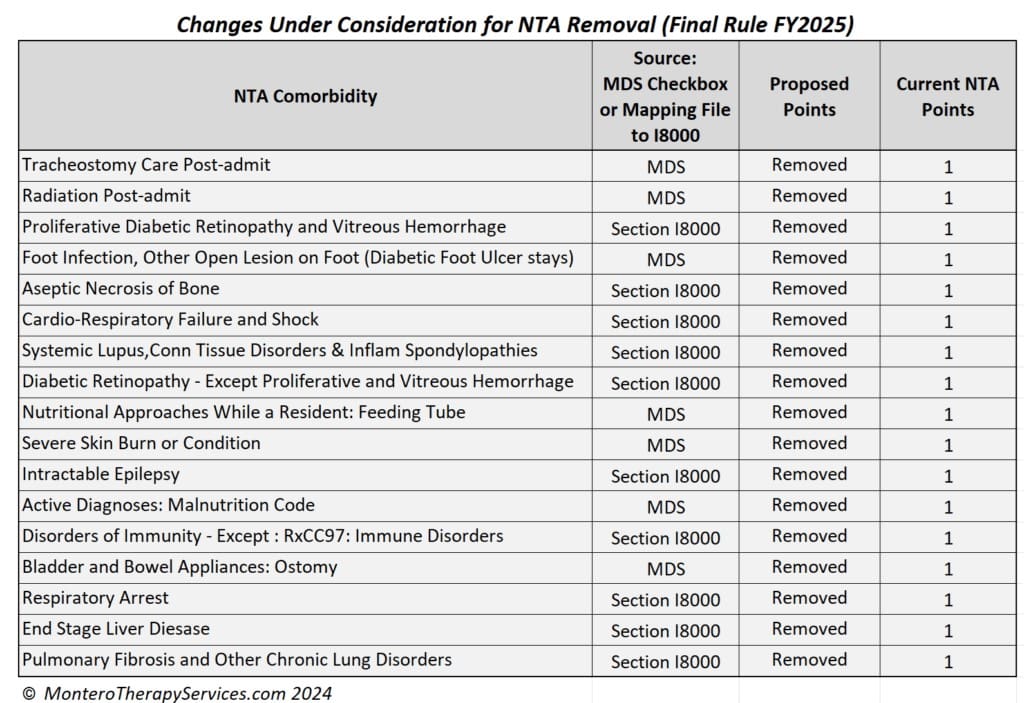
What will the impact be of these NTA point removals?
The original CMS NTA Fact Sheet states that “classification is determined by the presence of certain conditions or the use of certain extensive services that were found to be correlated with increases in NTA costs for SNF patients.“
When looking at the list of NTA points being removed, the question becomes “what about the increased costs associated with them?”
Again, no changes go into effect 10/1/24…these are something to look forward to for the future.
mDS Changes
The RAI Manual has been updated for 10/1/24 with the expected changes as follows:
- Removal of Section GG Discharge Goal items for Self Care and Mobility, leaving only the “Performance” column. The DC Goal items were the ones that could have a “dash” without a potential payment penalty. With this now gone… no GG dashed items!
- Section GG coding tip updates for stair questions
- Section I Coding Septicemia 12100 – Criteria Specified
- Section K Feeding Tube definition clarified
- Section K IV Fluids definition updated to included “nutrition and/or hydration”
- Section N addition of Anticonvulsant to list of High-Risk Drug Class Use & Indication
- Section O update of IV Access definition to exclude AV fistula
- Section O Pneumococcal Vaccine clarification
- Section O0350 New Question “Resident COVID-19 Vaccination is up to date”
- Chapter 5 Change on Correction of MDS Assessments (explained below)
Changes in Chapter 5 include instructions on how to handle deletion of a MDS that was completed for purposes other than OBRA or PPS, and was submitted to iQIES in error.
Our chart reviews indicate this happens frequently…. a PPS 5-Day assessment was completed for a Managed Medicare plan but should not have been submitted, and was sent accidentally.
Because a modification or inactivation does not completely remove the record from iQIES (it is archived in a history file), a “manual deletion” may be required, which is accomplished by contacting the facility’s State Agency to request an Individual Assessment Correction/Deletion Form, to manually delete all traces of the record from iQIES. It’s not as simple as it used to be!
The policy and procedures for a Manual Correction/Deletion Request are provided in Chapter 5 of this Manual. Here is the new language:
A Manual Deletion Request is required only in the following four cases:
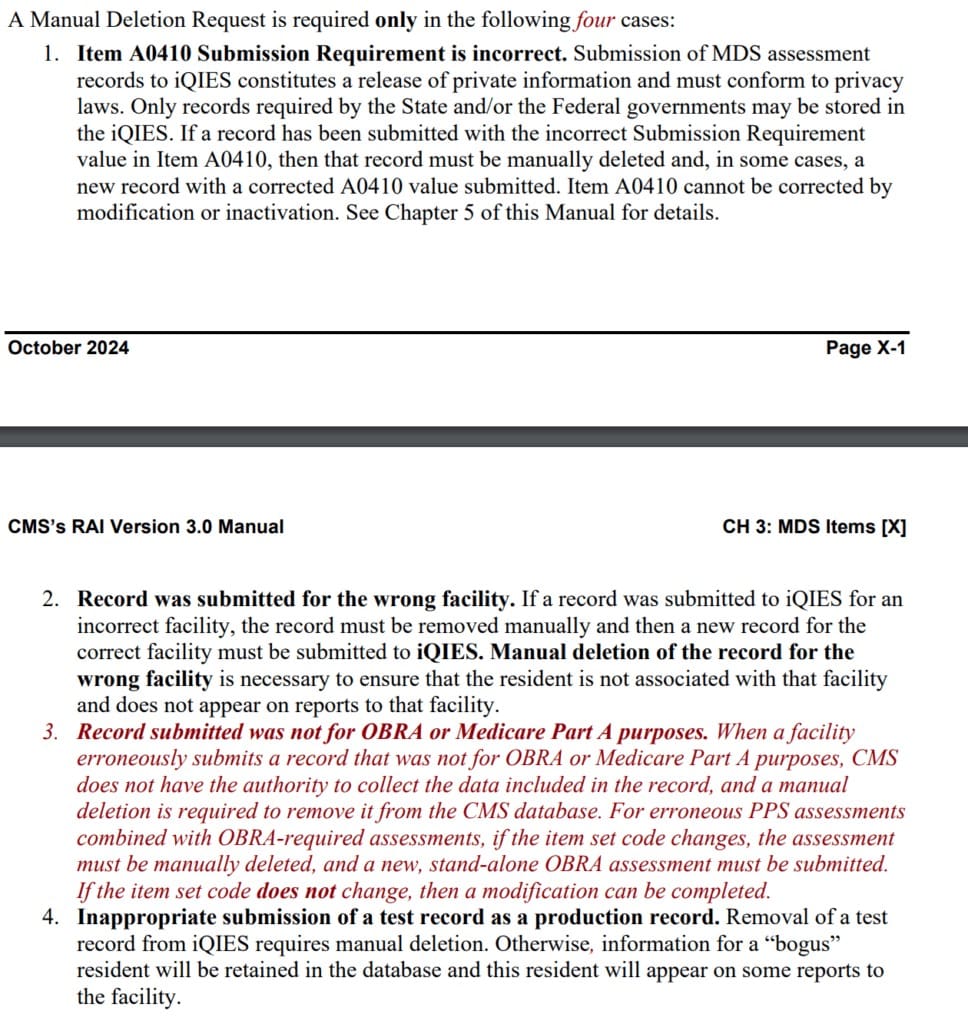
Based on the new language, the process will be dependent on if the item set changes:
- A PPS 5-Day combined with an OBRA Admission, submitted for a resident that did not have traditional Medicare Part A, could be modified the “old fashioned” way.
- A stand-alone PPS 5-Day submitted for a resident that did not have traditional Medicare Part A, would require contacting the State Agency to request a manual deletion.
Here is the link to the update RAI Manual. All items in red identify what’s new.
https://www.cms.gov/files/document/finalmds-30-rai-manual-v1191october2024.pdf
MDS Changes for 10/1/25
Effective on the 10/1/25 5-Day PPS Assessments, these items will be removed from Section O:
O0400.A, B, C: Speech, Occupational and Physical Therapy:
- Individual, Concurrent, Group, Co-Treatment Minutes
- Days
- Therapy Start Date and Therapy End Date
O0400.E.2. Psychological Therapy; Days.
The Final Rule included CMS’ response to multiple comments submitted identifying concern with removing these items. CMS indicated these MDS items are not needed to determine PDPM payment, and removal of the items decreases the “burden” on those completed the MDS by “6.6 minutes.” CMS reminds us that therapy services for the entire Part A stay are included on the PPS Discharge MDS, and will identify changes in service provision.
CMS acknowledged the reduction of therapy service volume and intensity since the start of PDPM, though reiterated that the impact on resident function is the bottom line, and Measures are in place to monitor this. CMS gave the example of the Discharge Function Score as one of the indicators used to determine progress under Medicare Part A.
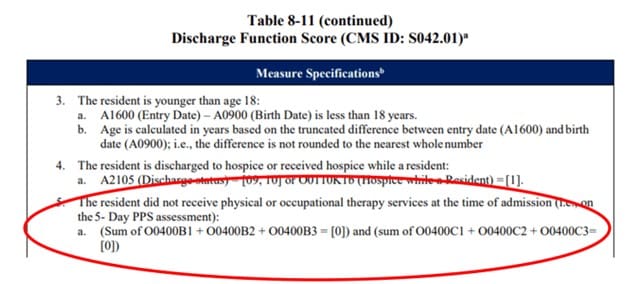
As of this date, the Discharge Function Score Measure uses the “PT and OT Therapy Items” from the PPS 5-Day to determine if the resident should be excluded from the Measure or not, so if these items are being deleted from the MDS, we would expect to see a change to the “List of Exclusion” shown below. Not every PPS day 1 will have an admission MDS tied to it.
Insert Deep Breath Here….
Changes To CMS Medicare Part A Quality Measure Programs
If you are not already heavily involved in your SNF Quality Measure Program processes, NOW is the time. As these Measure Programs grow and grow, don’t get left behind. By understanding the Measures and Programs, SNF therapy and MDS professionals can be a godsend to their facility. Here, we break down what will be changing in the SNF QRP and SNF VBP Programs.
SNF Quality Reporting Program – SNF QRP
The SNF QRP is the program that started small over 8 years ago [remember when Section GG was new?] and is now ballooning into the program with the most measures. This is a pay for reporting program, meaning, SNFs are required to report measure data, and if not reported, facilities will be subject to a 2% Part A payment penalty.
The penalty occurs when information is missing, not for poor outcomes. [yet]
What does missing data look like? MDS questions that have (dashed) data in select items, or information that is required to be provided directly from the SNF to the CDC’s National Healthcare Safety Network (NHSN), both count toward “missing data.”
Here is a link to all the MDS questions that, if not filled out, will trigger the payment penalty if the threshold is met. This list is in effect through the end of 2024.
The FY2027 APU Table has the MDS questions for CY 2025
For the present CY2024 collection period, both the current MDS and the MDS with updates due 10/1/24 are in play. The list of item sets (MDS questions) continues to grow, making the attainment of submitting100% data on 90% of all Part A MDSs a challenge.
Make sure MDS staff have the list of MDS items above. These are the MDS items being collected NOW that will potentially impact FY 2026 Annual Payment Update (APU) Determination.
Here are the 15 Measures in place for FY2025
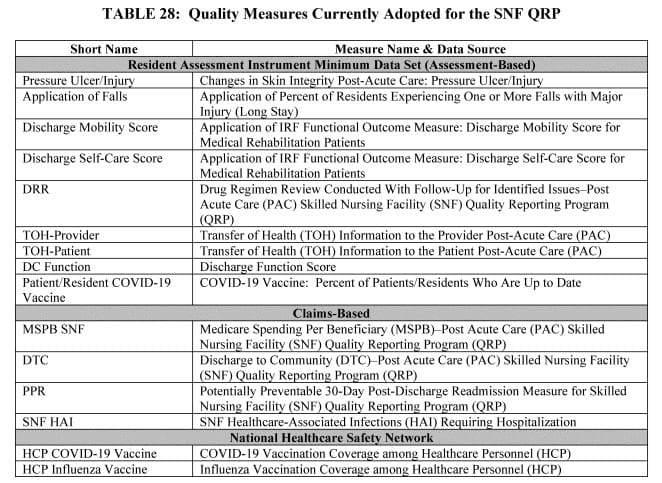
The list is a little shorter this year due to the removal of 3 Measures that involved Section GG:
- Admission and Discharge Functional Assessment /Care Plan That Addresses Function – Requiring 1 Discharge Goal
- Change in Self-Care Score
- Change in Mobility Score
But don’t worry, the Measures that were approved in the prior year are now on the list:
- Discharge Function Score Measure
- Outcome measure from Section GG Self Care and Mobility Technical Report
- Calculated % of Part A residents who meet or exceed DC Function Score
- Uses 10 GG items: Eating, Oral Hygiene, Toileting Hygiene, Roll L/R, Lying to Sit, Sit to Stand, Transfer, Toilet Transfer, Walking 10′ and Walking/Wheeling 50′
- Data collection started 10/1/2023
- COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) Measure
- Report the number of HCP who are up to date with recommended COVID-19 vaccinations
- Data collection started 10/1/23
- COVID-19 Vaccine: Percent of Residents Who Are Up to Date
- Data collection starts 10/1/24 with the addition of new MDS question to capture the data
Newly Proposed measures….
CMS is not adopting any “new” SNF QRP Measures in the Rule. However, there are some changes to be aware of with “existing” measures, including new MDS data elements (questions).
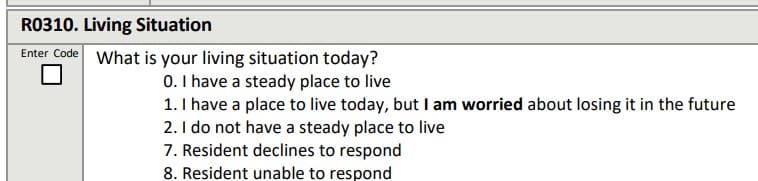
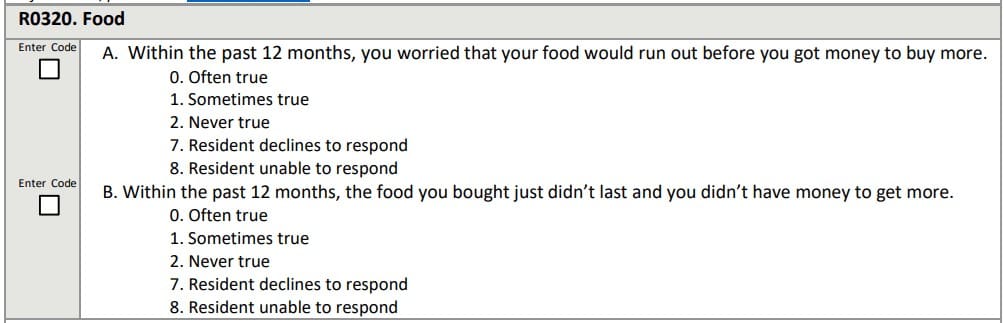
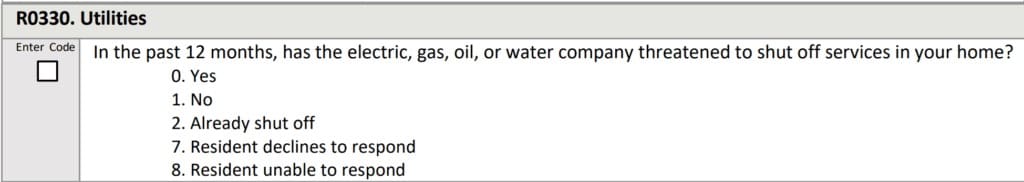
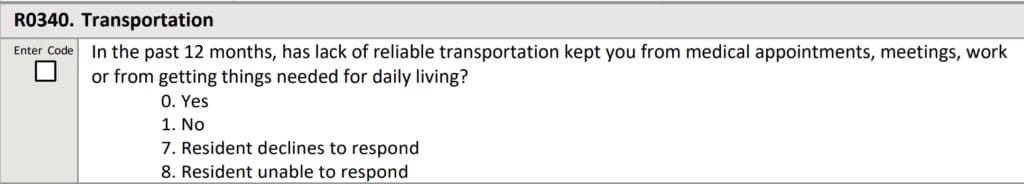
CMS is proposing to add 4 new items as Standardized Patient Assessment Data Elements (SPADES) under the Social Determinants of Health (SDOH) category, and modifying 1 existing element.
SDOH are defined as the socioeconomic, cultural, and environmental circumstances in which individuals live that impact their health. SPADES are the data elements (MDS item questions) that are standardized across all post acute care settings (ie: Home care, Inpatient Rehab, SNF). For example, this is why we see GG Items collected in multiple settings.
Data collection for these items would be for new admissions only beginning 10/1/25 through 12/31/25, once these items are added to the MDS, with a payment impact in FY2027.
The 4 New MDS Questions – Future Medicare pPS 5-day
Below are the 4 new items, each proposed to collect information on admission, that will allow the SNF to collaborate with additional agencies for support of the resident upon discharge.
Living Situation:
Food (x2):
Utilities:
1 Modified MDS Question on Future Medicare PPS 5-day
CMS is modifying the existing Transportation Item in Section A1250 to clarify a look-back window and simplify the response options. This item is proposed for FY2027 for new admissions starting 10/1/25 only, no longer requiring completion at discharge, and will move from Section A of the MDS to a new “Section R.”
Greater Chance for 2% Payment Penalty
As of 1/1/2024, the required MDS data reporting threshold increased from 80% to 90%. This means CMS requires SNFs to report 100 percent of the required quality measures data and standardized patient assessment data collected on at least 90 percent of all PPS Part A assessments, with a payment penalty kicking in 10/1/25 if not followed.
The SNF QRP works in 2 timetables. The collection of data NOW [reporting period] will impact your payment in the FUTURE.
As the list of measures continues to grow, there is a greater chance of missing information and incurring a 2% payment penalty. Not only do 90% of MDS assessments need to contain 100% of the SNF QRP required data from the MDS, SNFs also need to submit 100% of data for the COVID-19 and Influenza Vaccination for Healthcare Personnel to the CDC NHSN system. If info is missing either way, the penalty will apply. This does not leave much room for error.
….and as we dig into additional SNF QRP changes next, there will be 1 more variable to add to the list of things that can trigger the 2% Part A payment penalty.
Future Validation Process of SNF QRP Measures
SNF QRP Measures require validation and CMS is proposing methods to validate both the MDS and Part A claims data beginning FY2027. The Rule outlines a process using a validation contractor that will request up to 10 records per year from 1,500 SNFs, aligning the QRP record review with the VBP review so the same residents are used for selection.
Records beginning on 10/1/24 through 9/30/25 would be selected for the FY 2027 validation process (impacting payment FY2027 or 10/1/26). Failure to submit records within 45 days of the request will result in a future (2 years out) 2% Part A payment penalty….so we can add this to the list of existing items that trigger a 2% payment penalty!
The Rule also confirms a future MDS validation review process to determine if what is coded on the MDS is supported in the record, to not only validate QM triggers, but potentially challenge PDPM reimbursement items (….like the 5-Record TPE Audits all SNFs had…only expanded ….and permanent). CMS intends to propose a methodology for validating the medical records against the MDS in future rulemaking prior to the start FY2027 [even though the medical records for that FY will be from records in FY 2025…. which starts on 10/1/24!]
On to the last quality measure Program….
SNF Value-Based Purchasing Program (SNF VBP)
The SNF VPB Program works by reducing Medicare Part A payments to ALL SNFs by 2% and then allows for an opportunity to recoup part (50-70%) of the 2% by demonstrating success with the established Measure. These “incentive payments” are intended to encourage SNF improvements in the quality of care provided to Medicare beneficiaries.
Since the start of this Program, there has only been 1 Measure: The SNF 30-Day-All-Cause Readmission Measure, which looks at if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital to the SNF.
Though there are no new measures in this year’s Final Rule, we are still impacted by the multitude of new measures added over the past 2 years that are now kicking in 10/1/24.
In addition to the only Measure currently in play (#1 on the list below), this is the full list of adopted Measures:
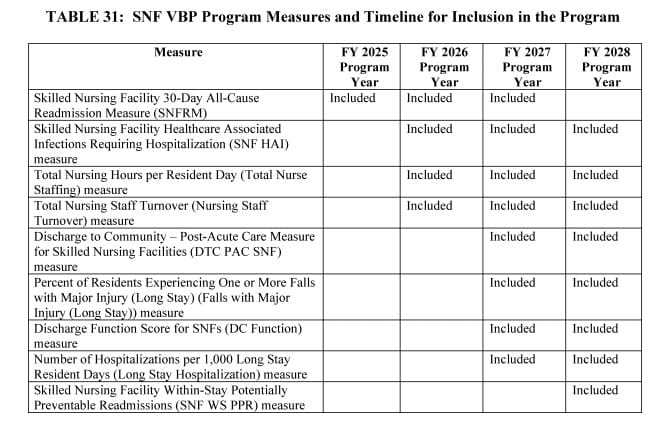
Performance period data collection began on 10/1/23 (FY2024) for Measures 2-4 on the list below. The Program Year is typically 2 years after the Performance Year, so attention needs to be paid to the Performance Year when the actual data is collected.
When the Program Year hits, it’s too late to do anything about the data as it was collected 2 years prior! Payment impact is based on the facility’s performance 2 fiscal years prior.
Measures 5-8 on the list above are waiting on deck with data collection to start 10/1/24 (FY2025), with a payment impact 10/1/26 (FY2027).
- Discharge to Community (DTC)
- Claims based Measure for % of short stay Part A residents discharged to community within 100 days of admission, with no hospital admission for next 30 days
- Also SNF QRP, 5-Star and publicly reported
- Falls with Major Injury (MDS Measure includes long-stay residents)
- Already a QM in other programs, used in 5 Star and publicly reported
- Discharge Function Score (MDS Measure)
- % of Medicare A stays that meet or exceed an expected DC Function score, using 10 Section GG items: Eating, Oral Hygiene, Toileting Hygiene, Roll L/R, Lying to Sit, Sit to Stand, Transfer, Toilet Transfer, Walk 10′ and Walk 50′/Wheel 50′
- Same Measure from SNF QRP, 5-Star and publicly reported
- # of Hospitalizations per 1,000 Long Stay Resident Days (Claims Measure)
- Already publicly reported and used for 5 Star
- Data collection starts 10/1/24
The last Measure on the list, SNF Within-Stay Potentially Preventable Readmission Measure (SNF WS PPR) is a claims measure that will replace the 1st Measure on 10/1/27 (FY2028) and will use the performance period of both FY2025 and FY2026…. so even though FY2028 is a long way away, data from 10/1/24 will be used to calculate performance.
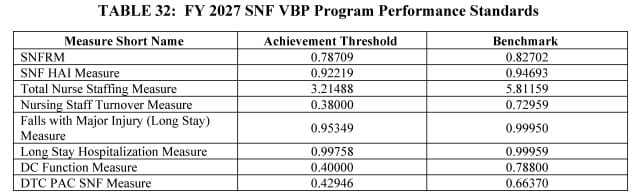
SNF VBP Measure Performance Standards
The Final Rule released the Achievement Threshold and Benchmark for each of the VBP Measures as shown below.
Are we done yet???
We are almost there….. lots of information to get through every year!
Though we will not go into the details here, it is important to know that the Final Rule has a full section dedicated to Nursing Home Enforcement, outlining “the Biden-Harris Administration commitment to ensuring that all residents living in nursing homes receive safe, high-quality care.” The Final Rule gives CMS greater flexibility by removing some restrictions on how rules are enforced, including Civil Monetary Penalties for health and safety violations, etc. This portion of the Rule has created quite a stir and it is recommended that therapy and MDS staff gain more insight on this topic by speaking with your administrative team.
In Summary…
October 1st is always about change for SNF therapy and MDS professionals… and it hasn’t killed us yet!
This resource was surely the “long answer” to what’s changing 10/1/24. So what’s the “short answer?”
- Part A rates will go up 4.2%, which is a minimal increase per SNF
- Case Mix Group CMI values will stay the same as last year
- The Wage Index was shuffled a bit, reclassifying multiple locations
- PDPM Mapping changes are minimal…. only 4 code changes
- No NTA changes will happen this year. Maybe next year?
- MDS changes are minimal
- SNF QRP 15 Measures are in play with no new ones proposed
- There is a much greater chance to incur a Part A 2% payment penalty as the list of requirements keeps growing, and now includes failure to timely respond to a QRP audit
- SNF VBP has no new measures, however, 4+ Measures kick in for data collection on 10/1/24 that will impact future Part A payments.
That’s the long AND the short of it!
Print it, save it, and go enjoy the rest of your Summer!
If you have any questions, send them to our Just Ask Q&A Team .
Thank you for ALL you are doing to provide the BEST CARE to the geriatric population!
Important Resources to Bookmark:
HERE is a link to the Final Rule. PDF Version
HERE is a link to the CMS Fact Sheet.
Here is a link to the updated RAI Manual.
PDPM Calculators and Resources HERE
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
President | Montero Therapy & MDS Resource Team
Join Us: September 25th @ 12 pm: SNF Rule Changes For Medicare Part A & Part B 10/1/24-12/31/25
Every October 1st the Medicare Part A Rules change…..PDPM, Reimbursement, MDS….
Every January 1st the Medicare Part B Rules change…. Reimbursement, Coding, Modifiers….
Change is inevitable in the SNF!
Stay up to date on rule changes that impact your practice.