Hoping ICD-10 would just go away?
Just wating long enough for someone else to figure it all out and then pass it on to you?
Well if you answered “yes” to the first question, I’m right there with ya! If you answered “yes” to the second question:
- You’re pretty smart {and brave}, and
- Today is your lucky day! {Did you think we would let you down?}
The ICD-10 transition is a few days away but it is not too late to get the information you need to make the transition in long-term care without missing a beat! Spend a few minutes here today and you will walk away a happy coder! We will review the upcoming changes, what you will need to do differently starting October 1st, and provide you with info you can use as a starting point.
The Details
What: The transition from ICD-9 to ICD-10. More specifically, the International Classification of Disease, Clinical Modification, 10th Edition, ICD-10-CM
When: Starts for dates of service on or after October 1, 2015. ICD-10 has been in use by other countries since 1998. The US mandated the replacement of ICD-9 to ICD-10 with a start date of 10/1/13; however, implementation has been delayed for 2 years. No more delay…it’s here!
Where: Here! In the USA for all HIPAA-covered entities. So, entities like Worker’s Comp and No-fault may continue to use ICD-9, though CMS has strongly encouraged the transition for these entities as well because the ICD-9 Database will no longer be maintained. We may see the non-HIPAA entities lagging, which is going to make our billing challenging in certain scenarios.
Why: Greater specificity in coding is needed with the goal of improvement in healthcare delivery and policy decisions. The change will allow for improved data capture, quality reporting, data analysis and research.
How: Well, this part needs a bit more explanation…so let’s start…
A New Cast of Characters
There are {a ton} more codes. The number of CM Codes, or Diagnosis codes, jumped from 14,025 with ICD-9 to 69,823 with ICD-10. PCS Codes, or Procedure codes, jumped from 3,824 with ICD-9 to 71,924 with ICD-10. The CM codes are the ones we will be selecting in LTC – the PCS codes are “procedure codes” and are for use in the inpatient hospital setting. ICD-10-PCS is a replacement for ICD-9-CM, Volume 3. Our patients will come to our facilities from the hospital with these codes, but these are not codes we will ever have to assign. {Thankfully!}
So for the rest of the Blog, let’s put the 71,924 ICD-10-PCS codes away and focus on the 69,823 ICD-10-CM codes we will need to get to know and love. I guess that is greater specificity for you!
Code Structure:
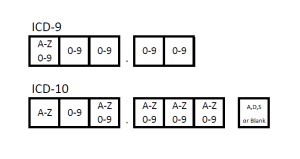
- ICD-10-CM codes will be:
- 3-7 characters in length
- The first character will always be a letter
- The second character will always be a number
- The remaining characters can be either a letter or number
- The 7th character will be a letter, but should be left blank if not required
Code Organization:
CMS has provided the full listing of codes in alternate formats, so if you did not purchase a ICD-10-CM code book yet, you really don’t need to. You can save both of the links provided here to your desktop and access them as needed. The first format is a Tabular List of Diseases and Injuries. The list is organized into 21 “Chapters” and each Chapter is dedicated to a unique set of injury or disease. Each injury or disease set within a Chapter is categorized by a letter. So for example, Chapter 1, “Certain infectious and parasitic diseases” has all the “A” and “B” codes. Chapter 2, “Neoplasms,” has the “C” and “D” Codes. Remember, the first character in ICD-10 is always a letter…so get to know your letter!
Click here for the ICD-10-CM Codes listed by category (Tabular List of 21 Chapters)
Common chapters for therapy will be:
- 6 – Diseases of the nervous system (G00-G99)
- 13 – Diseases of the musculoskeletal system and connective tissue (M00-M99)
- 19 – Injury, poisoning and certain other consequences of external causes (S00-T88)
- 20 – External causes of morbidity (V00-Y99)
The second format provided by CMS is an Index to Disease and Injuries. This list is organized alphabetically by key words and is intended to provide a cross-reference to the Tabular List. Once the key word with code is located in the index, a search of the code in the Tabular List will then provide additional information as to if a seventh character is needed, etc.
Click here for the ICD-10-CM Codes listed in Alphabetical Order by Index of Disease and Injury
7th Character:
A 7th character is not always required. The Tabular Index will indicate if required at the beginning of each new code section – and this requirement is common for Chapter 19, the Injury category. If a 7th character is not required, don’t fill it with a “0” — just leave it off the end or your code will be invalid and may cause a denial. If you have looked at the Tabular Index and noticed that some of the codes require a 7th character, but the code itself is less than 6 characters, you may have wondered how to complete this task. In cases like these, you will need to use an “x” as a placeholder. For example, S47.1 is the code for “Crushing injury of right shoulder and upper arm.” It is only 4 characters, but requires a 7th character. In this case, the code would look like this: S47.1 x x A.
So what is the 7th character? It is a letter, most often an A, D or S (though could be others), each with a specific definition.
- “A” designates the Initial Encounter and describes the period of active treatment for the injury
- “D” designates the Subsequent Encounter and describes the period of routine care for healing and recovery, after active treatment is complete
- “S” designates a Sequela and indicates a complication or condition that arises later (ie: late effects)
A patient may be admitted with a code designating “A” as the initial phase, and the therapist may need to modify that diagnosis code to reflect a 7th character of “D,” indicating a new phase of the injury recovery process. The physician will not likely take the initiative to make this change – thus making it the responsibility of the therapist.
External Cause Codes:
Chapter 20 contains codes called “External Causes of Morbidity (V00-Y99)” These codes classify environmental events and circumstances as the cause of injury, and other adverse effects. Where a code from this section is applicable, it is intended that it shall be used secondary to a code from another chapter of the Classification indicating the nature of the condition. Most often, the condition will be classifiable to Chapter 19, Injury (S00-T88). Codes from Chapter 20 should be used to provide additional information as to the cause of the condition. These codes can answer questions regarding how the injury happened, the location of where it happened and if it was an accident or not.
Therapy Treatment Diagnosis
So, if you thought that all you needed was a new list of codes to replace the old ones, you thought wrong. Unfortunately, this is not a 1 for 1 transition. Because of the greater specificity of the new codes, the old codes will need to be paired up with, in some cases, multiple potential new matches, and then the most appropriate code will need to be determined based on the clinical condition. This applies for almost all of the “treatment diagnosis” codes that therapists pick. Remember,the treatment diagnosis is the code that represents the condition that therapy is treating, where the “medical diagnosis” is the code that typically comes from the physician or the hosptial discharge summary. So for all the ICD-9 treatement diagnosis codes out there currently in place, there may be a potential match of multiple ICD-10 codes.
For example, gait dysfunction {ICD-9 = 781.2} now has at least 4 potential matches to select from, and only a therapist could make that selection based on specific knowledge of the patient. Which one would you pick?
| ICD-10 CODE | ICD-10 CODE DESCRIPTION |
|---|---|
| R26.0 | Ataxic gait |
| R26.1 | Paralytic gait |
| R26.89 | Other abnormalities of gait and mobility |
| R26.9 | Unspecified abnormalities of gait and mobility |
Muscle weakness {ICD-9 = 728.87} presents with 1 main match, but offers no specifity as to what is weak and why. In cases where “M codes” from Chapter 13 are used, additional treatment diagnosis codes will be expected to be used to support these codes. More specific codes were not available using ICD-9. Chapter 13 Diseases of the musculoskeletal system and connective tissue (M00-M99) states that use of an external cause code following the code for the musculoskeletal condition, if applicable, is needed to identify the cause of the musculoskeletal condition. External Cause codes (V00-Y99) are from Chapter 20.
| ICD-10 CODE | ICD-10 CODE DESCRIPTION |
|---|---|
| M62.81 | Muscle weakness (generalized) |
Common Therapy Codes for PT, OT, SLP
CMS provides a neat code “look up” tool to help sort through the information. Click here for the link. Here are some of the ICD-10 codes for common PT, OT and SLP treatment diagnoses in the long-term care setting:
- PT {781.2 / 719.7}
- R26.0 Ataxic gait Staggering gait
- R26.1 Paralytic gait Spastic gait
- R26.2 Difficulty in walking, not elsewhere classified
- R26.8 Other abnormalities of gait and mobility
- R26.81 Unsteadiness on feet
- R26.89 Other abnormalities of gait and mobility
- R26.9 Unspecified abnormalities of gait and mobility
- OT {728.87 / 780.99 / 781.3 / 781.92}
- R53.1 Weakness
- R53.81 Other malaise / Chronic debility / Debility / General physical deterioration
- R27.9 Unspecified lack of coordination
- R29.3 Abnormal posture
- SLP {787.20-787.24}
- R13.10 Dysphagia, unspecified
- R13.11 Dysphagia, oral phase
- R13.12 Dysphagia, oropharyngeal phase
- R13.13 Dysphagia, pharyngeal phase
- R13.14 Dysphagia, pharyngoesophageal phase
How Will This Impact Billing and the MDS?
In the SNF setting the ICD-10 codes are needed on the UB-04 billing claim for Part A and Part B. ICD-10 codes will also be required on the MDS. For Part A and Part B billing, the dates of service on or after October 1st will require the new codes. MDS’s with the ARD of October 1st or later will require ICD-10 codes in Section I. Facility billing, if not already done monthly, will need to be split to ensure ICD-9 codes are on September dates of service and ICD-10 codes are on October dates of service, otherwise, claims will be denied. CMS, after pressure from the AMA, issued a statement indicating that the transition will include a “grace period” in which claims will not be denied soley on lack of specificity, as long as the correct 3 digit “family of codes” is used. You can read the original letter from CMS here and the clarifying letter from 9/2015 here.
Our Recommendations
It’s never too late to get on board with change. Here are the key items that you should make sure you have covered:
- Save the CMS Tabular, CMS Index, and CMS code look-up links to your desktop for easy reference
- Don’t rely on Apps for the conversion
- Convert all ICD-9 codes (medical and treatment diagnosis) to ICD-10 using the most specificity possible
- Select additional ICD-10 codes to support your treatment diagnosis as needed
- Ensure the ICD-10 codes have the 7th digit or place holders if required
- Communicate with your billing department and MDS Coordinator to ensure a smooth transition for Part A and Part B claims
If you have specific questions, need more information, or want to take advantage of the coding work that Montero Therapy has already done, join us this Tuesday, September 29th from 3:00 – 4:00 pm EST for a 1 contact hour approved Webinar. We will provide greater detail to the information here, as well as provide participants with PT, OT and Speech code-specific information that you can save and print for your clinic to help get you started.
Check out this COURSE on ICD10 Coding for the SNF Therapist
Also, our Just Ask! Q&A Forum is available if you have any questions.
Happy coding!
In Your Corner,
Dolores
www.MonteroTherapyServices.com




2 Comments