
Has CMS signed off on sNF Therapy?
Skilled Nursing Facilities (SNF) across the country have been preparing for months for the major changes set to hit October 1st. The Federally required Minimum Data Set (MDS) data collection tool was bringing with it the biggest change in decades and after months of training, MDS nurses and therapy staff were ready.
But with the October 1st roll-out came huge disappointment to find out that Center for Medicare and Medicaid Services (CMS) snuck in some unexpected changes to the data collection tool, in particular, a change involving therapy days and minutes. And maybe it feels as though this change snuck up on us because we were preoccupied with the bazillion other changes that would kick in on October 1st… you know….the shift from Section G to GG, new interview questions, and the 200+ other new MDS items, to name a few. Nonetheless, this therapy change happened.
The October 1st roll-out also brought with it too many Electronic Medical Record glitches to count, all resulting from the multitude of changes to the MDS tool. Providers reported missing questions, the inability to fill in data, skip patterns out of whack, and fatal errors on attempted submissions. It was initially thought that the inability to enter therapy days and minutes was possibly part of this major glitch.
No such luck.
what was the change?
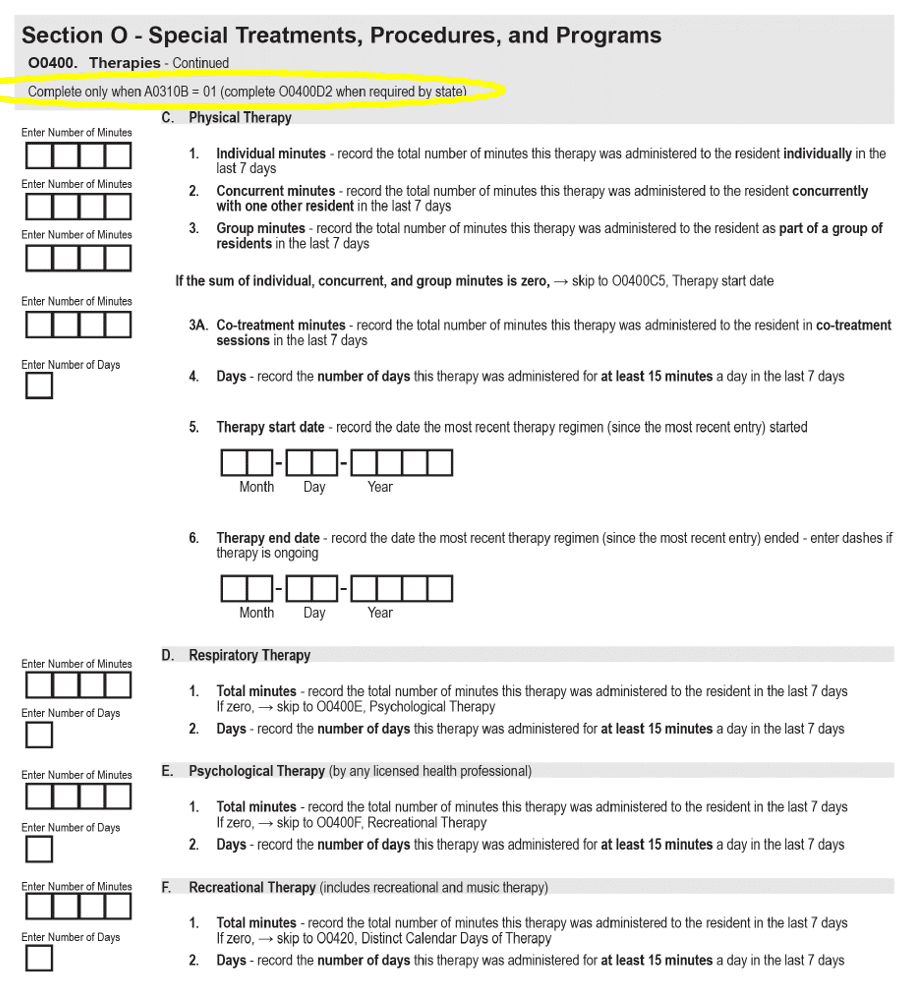
Section O0400, “Therapies,” which includes data collection for Physical, Occupational and Speech Therapy, as well as Respiratory, Psychological and Recreational Therapy, was removed from all MDSs with the exception of the 2 Medicare Part A assessments (5-Day and End of PPS). Section O0400 included items such as Therapy Start Date, Therapy End Date, Type or Mode of Therapy (Individual, Group, Concurrent), Total Days and Total Minutes. Mind you, this is a veteran section, that has been on the MDS for decades.
Neither the Draft Version of the new RAI Manual for the MDS 3.0 version 1.18.11 nor the Final Version of MDS Item Sets in April, mentioned removing Section O0400, “Therapies” from the Admission, Quarterly, Annual and Significant Change OBRA assessments.
Possibly the confusion came from the subsequent release of 4 additional revisions of the “Final” Item Sets between April and July, until the final-Final version, v5, was released in August. Somewhere along the way, Version 3 to be exact, CMS released a revision of what the MDS Items sets would “look like.” In this version, there was a tiny addition of text noted in the screenshot to the instructions of Section O0400, Therapies.
Now, unless you have a copy of the MDS handy when reading the additional text below circled in yellow, or happen to know all the MDS question numbers by heart, this small text addition may not seem like a big deal. But what this text says is that the therapy information will no longer be collected unless the MDS-type is a Medicare Part A 5-Day PPS MDS (a.k.a. A0310B=01).
Faced with this change now after October 1st, many are wondering what could possibly be the rationale behind discontinuing a Section that has been on the MDS for over 20 years that provides valuable data about therapy services for the majority of residents in the SNF?
Yes, therapy information will still be collected for Medicare Part A stays, but these residents only make up a small percent of the 1.2 million residents in SNFs throughout the country, as identified here by KFF.
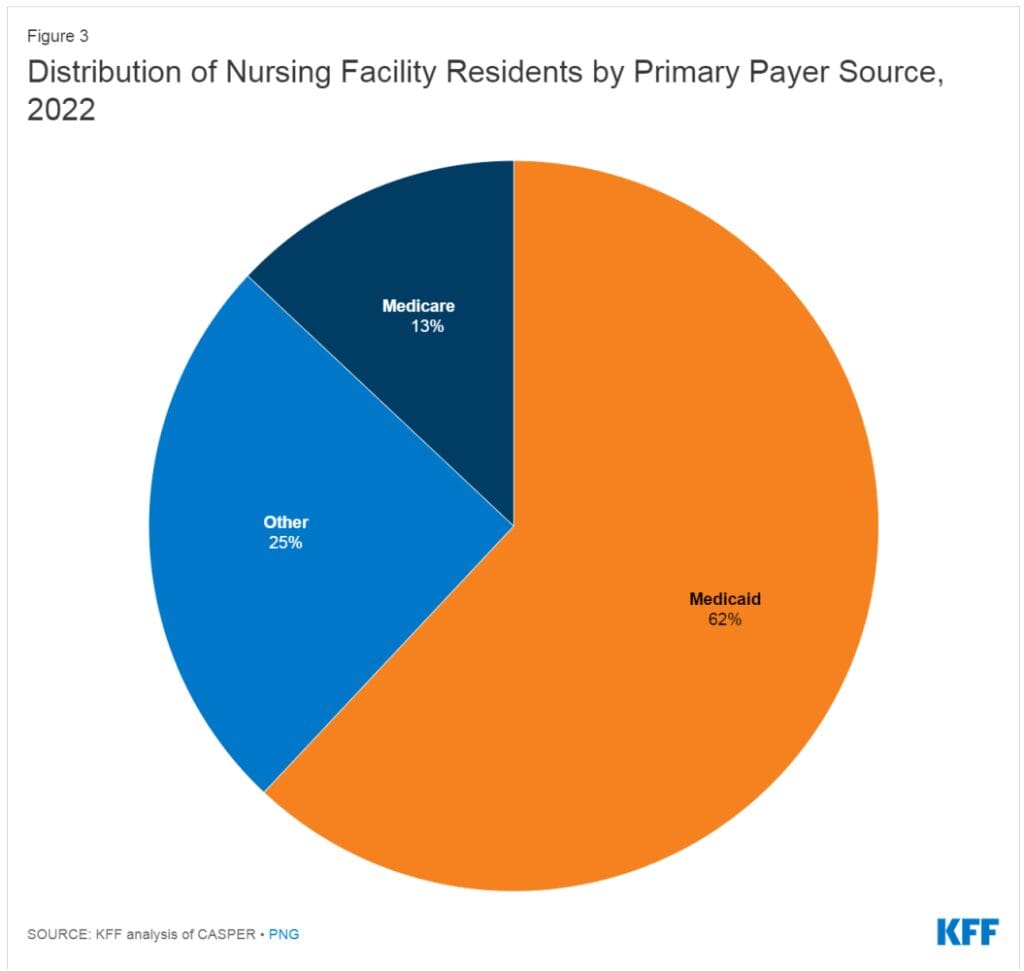
What about the other 87% of SNF residents? Don’t the therapy days and minutes matter for the majority?
What’s the big deal?
This tiny change in text will have a big impact, both now and in the future.
Here are just a few off-the-cuff implications of no longer collecting therapy days and minutes data on the Admission, Quarterly, Annual and Significant Change MDS (OBRA) assessments:
- CMS will have no way to track the total number of long-term care residents receiving therapy services, including the amount of therapy, frequency and duration of the service.
- CMS will no longer be able to see changes in therapy practice patterns in non-Part A residents.
- CMS will have no data from residents with a primary payor other than Medicare Part A (Medicare Advantage, Medicaid, private pay or other non-Medicare Part A payor) to be used to compare and contrast with Medicare Part A. Wouldn’t CMS want that data as a comparison at the very least?
- Do Medicare Advantage residents receive less therapy than traditional Part A? Would have been pretty easy to get that information from a snapshot of MDS data!
- CMS will have no insight into residents who trigger for short and long stay quality measures involving ADL decline, and if the decline (or improvement) could potentially be related to therapy services.
- Were the residents that triggered receiving therapy before or after the trigger?
- By discontinuing this data collection, CMS has effectively eliminated the possibility for all MDS-based research of the long-term care population to determine the benefits of therapy services on maintaining highest level of function, improving function, preventing contractures, reducing restraints, improving skin integrity…and the list goes on.
- Do long term care residents receiving therapy have fewer contractures, are they less prone to pressure ulcers? Getting this information won’t be so easy now.
Is it possible that at some future point in time, CMS may want to weave therapy services back in to a reimbursement structure? If so, CMS will wish they had this ongoing valuable collection of data. Ok, therapy may not see its way back into the reimbursement structure any time soon or ever, but it is still mind-blowing to think that continuing to collect data for this tiny section would be a burden.
With President Biden’s recent push to improve care and protect our seniors in long-term care facilities, why wouldn’t the inclusion of therapy data for long-term care residents of all payers across the country be important?
CMS needs to reconsider adding these data elements back to the Admission, Quarterly, Annual, and Significant Change OBRA assessments for all long-term care residents, as it is valuable information on so many levels, and it would seem to be in alignment with the buzz of nursing home reform out there.
There have already been 5 revisions to the “Final MDS” since the initial release earlier this year.
What’s one more?
Some advocacy, please
Now is the time to engage our professional associations, APTA, AOTA and ASHA, to advocate the importance of tracking and collecting therapy data for all residents residing in the 15,000 skilled nursing facilities across the country, not just those residents in a Medicare Part A stay.
And you too, Rehab Providers….. SPEAK NOW or FOREVER HOLD YOUR MINUTES.
In Your Corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
Montero Therapy & MDS Resource Team
MonteroTherapyServices.com
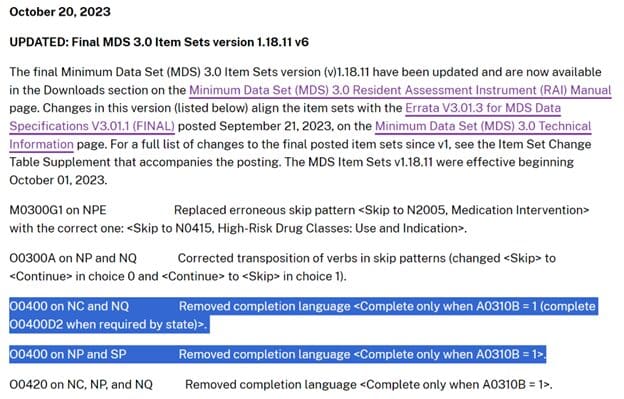
*11/1/2023 Update
I was waiting to see Section O therapy data back on all MDSs with my own eyes before saying “it’s back.” Thankfully, it’s back, with the CMS patch done on 11/1/23, retroactive to 10/1. Therapy data will once again be collected for all non-Medicare Part A residents. CMS posted the update on 10/20/23 to the RAI Manual home page, as shown below.
In Your Corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
Montero Therapy & MDS Resource Team
MonteroTherapyServices.com
