CMS released the Physician Fee Schedule (PFS) Proposed Rule last month, a.k.a. the “Medicare Part B Rule,” outlining changes for 1/1/25 that will go into effect unless modifications are made based on comments and feedback from providers due next week.
This 1,000+ page document includes information on payment rate changes, codes changes, supervision of assistants, telehealth and more! We highlighted the Medicare Part B rules that impact therapy in the SNF setting.
Proposed Changes For January 1st, 2025
1. Rate Information
Rate cuts for Part B have been the norm in recent years, and 2025 will be no different. CMS is proposing a 2.93% decrease in the average payment rate under the Physician Fee Schedule (PFS) as compared to CY 2024, according to the CMS Fact Sheet.
Rate cuts are due to a 2.8% Conversion Factor (CF) cut, the expiration of the 2.93% “intervention” from Congress implemented in 2024, and a positive budget neutrality adjustment of 0.05%.
The CF has not been trending in a favorable way over the past 6 years, and will drop from $33.29 last year to $32.36 for CY 2025. The CF, a value that CMS modifies yearly, is part of the formula that determines the dollar amount for each CPT code by converting Relative Value Units (RVU). The CF impacts all Current Procedural Terminology (CPT) Codes across the board. When the CF decreases, the overall payment rate for the CPT codes decrease, unless the RVU for a specific CPT code is increased enough to offset the CF drop.
Did you know you can look up any CPT code and check the reimbursement rate HERE ?
2. Modifiers And Manual Medical Reviews
KX Modifier Threshold
The “old” Therapy Cap is now disguised as the KX Modifier Threshold, and “threshold amounts” change yearly. The 2024 “threshold” of $2,330 for OT, $2,330 for PT and Speech combined, will increase to $2,410 for CY2025. Continued use of the KX modifier is required for all therapy services that “would have exceeded the previous therapy cap amounts,” or claims will be automatically denied.
The KX Modifier is an attestation by the therapist that the resident continues to require medically necessary services beyond the dollar threshold, and the rationale for the extended therapy services are documented in the medical record. All therapists should be aware of the amount of therapy a resident has received in a calendar year, and if over the threshold during a current episode of care, documentation should focus on supporting the extended services.
Manual Medical Review
The manual medical review threshold continues at the same amount of $3,000 until the next revision in CY2028.
This type of review is not automatic when the $3,000 is reached. CMS is uses the Targeted Probe and Educate (TPE) review process with providers identified through data submission as “outliers.” The TPE looks for providers with questionable practice patterns and provides training to decrease the error rate. For more information on the TPE process, visit the CMS info page or check out the Q&A Document.
3. Telehealth
As we are all well aware of, therapy professionals were not able to provide telehealth services prior to the Public Health Emergency (PHE) and are currently only able to provide telehealth now post-PHE, through a temporary continuation of these extended flexibilities outlined in the Consolidated Appropriations Act through12/31/24 for the SNF and other settings.
There are currently no active plans for an extension in place and on 12/31/24 telehealth under Medicare will end for therapy professionals, though a further extension is not impossible.
If, in fact, therapy professionals are able to provide telehealth beyond 12/31/24, there are 3 new codes in the Proposed Rule that will be added to the provisional list. These include last year’s new Caregiver Training Codes:
- CPT code 97550, face-to-face with caregiver, without patient present
- Initial 30 minutes
- Caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community
- CPT code 97551, face-to-face with caregiver, without patient present
- Each additional 15 minutes (used only after 97550 30-minutes is billed)
- CPT code 97552, face-to-face with caregivers representing more than 1 patient, without patient present
- Group caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community
Need a refresher on these? Click HERE.
Additional Telehealth Rule Updates for 2025:
Telehealth will continue on in CY2025, even if therapy professionals are not added as approved providers. However, if there happens to be an extension for therapy professionals, this will be important information to have. The Proposed Rule identified the following updates:
- Delivery requirements for Telehealth would allow the inclusion of two-way, real-time audio-only (vs the current requirement for audio-visual) communication technology for “any telehealth service furnished to a beneficiary in their home if”:
- The provider has the capability to provide 2-way audio-visual communications, though the inability to follow through is because of the patient. Meaning, “the patient is not capable of, or does not consent to, the use of video technology.”
- Modifier 93 must be appended to the claim for services described above to verify that these conditions have been met.
- The definition of Direct Supervision via telehealth to include audio-video communication “immediate availability” will be extended to 12/31/25, meaning “immediate availability” includes the use of audio/video, and need not be in person.
CMS has not yet provided an updated list of Telehealth CPT Codes for CY2025. Below is the current list of acceptable codes:
Download CY 2024 List Of Telehealth Acceptable CPT Codes
4. proposed changes to therapy-used cPT codes
Therapy Codes For Pay Increase
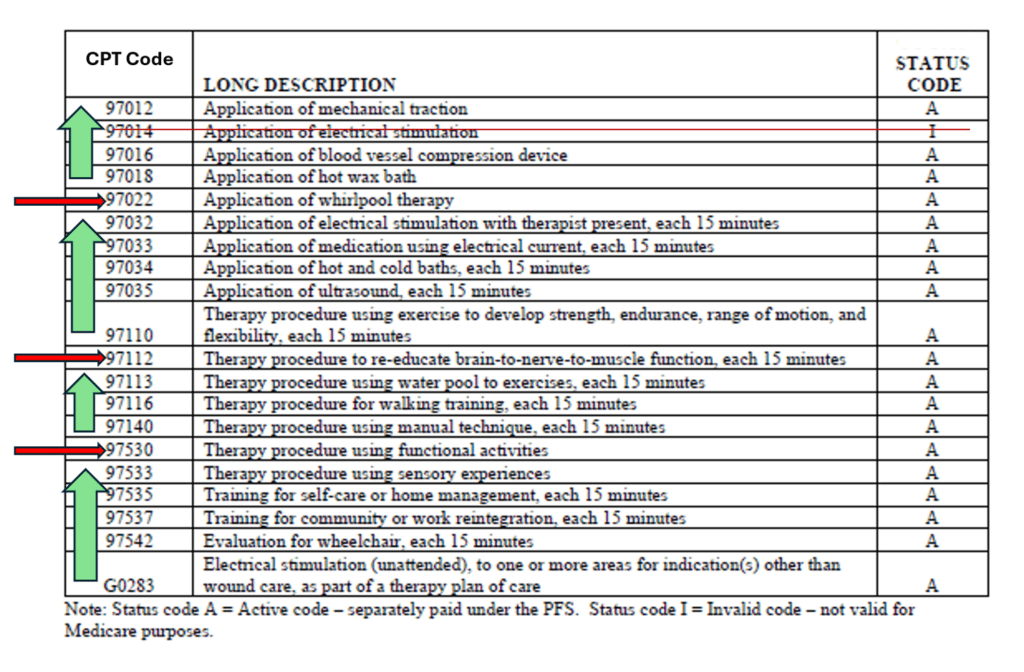
Professional Associations (APTA, AOTA) have been advocating for a review of “potentially misvalued codes” commonly used by therapy, to allow an increase in reimbursement. In the Proposed Rule, CMS agrees (finally) with updating the Practice Expense portion of the codes, which will change the reimbursement rates for the active codes below.
The results are an increase in 16 codes and decrease in 3 codes outlined below. Therapeutic Activities (97530), Neuromuscular Re-education (97112) and Whirlpool (97022) are the 3 codes proposed to have a reimbursement decrease, with all others showing an increase.
5. new rules for therapy practice
supervision of assistants redefined
The long awaited regulatory change updating the Medicare definition of Supervision of Assistants finally made the Proposed Rule. Though this rule change speaks to the private practice setting and not the SNF, it is too good not to include here (and some SNFs also provide outpatient therapy and this will impact them as well).
CMS is proposing to update the current definition in the private practice setting from “direct supervision” to “general supervision,” to align with the definition in other practice settings. In the SNF setting, Medicare Part A and Part B have defined supervision as “general” for decades, and now it’s time for the private practice setting to join in. If this makes the Final Rule cut, assistants in private practice will no longer need the supervision of the therapist to be “on site,” and will transition to the therapist being “immediately accessible.” This change will be for all settings where therapists independently bill Medicare for their services (outpatient, mobile home care, etc.).
This Medicare requirement update is a “reimbursement rule,” and does not change State Practice Act requirements. The requirements of your State Practice Act may be more strict than Medicare’s definition change. If your State Practice Act for your particular therapy discipline requires on-site supervision, the Medicare rule is overridden.
Also important to note, the temporary rule that has been in place since the start of the PHE that allows direct supervision via audio-visual technology, will remain through 12/31/25. This is the rule that allows the supervising practitioner be immediately available to engage via audio/visual technology, and “does not require real-time presence or observation of the service.”
plan of care requirements redefined
The current requirements from Chapter 15 of the Medicare Benefit Policy Manual for a physician certification of a Medicare Part B therapy plan of care require that the physician signs the Plan of Care within 30 days of the Initial Evaluation. If the plan of care is not signed timely, the certification requirement is not met, which is a condition for billing the services.
In the Proposed Rule, CMS is proposing to waive the requirement for signature on the Initial Plan of Care as long as there is a physician order or referral for the therapy services, and this is included in the medical record.
The updated rule would continue to require clinicians to submit the Initial Plan of Care to the physician, though signature requirements on this document will not be a contingency for billing the therapy services. There have been no proposed changes to the Re-Certification Process.
CMS is also seeking feedback on determining if there should be a timeline or deadline for a provider to make changes to the initial Plan of Care. This feedback will be considered in future rule-making.
Important Links And Resources
In Summary
Taking the good with the bad seems to be the theme of the Proposed Rule. Amidst rate cuts and the likely end to telehealth for therapy professionals in the SNF (though some swear this is good news), we have minimal coding changes, a payment increase on at least 16 therapy-used CPT codes, a more relaxed supervision requirement for assistants in the private practice setting, and the removal of the sometimes-headache of chasing down physicians to sign the initial therapy plan of care. Not too bad….
Remember, these changes are for Part B therapy only, and specific to the SNF setting. We teased out the parts of the Rule that applied to the SNF….so don’t worry about MIPS or other rules specific to private practice!
If you have comments for CMS regarding any aspects of the Proposed Rule, the submission deadline is coming up quick, 9/9/24.
As always, if you have any questions about the information or how it will impact you, send them to us here: Just Ask Q&A
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team
MonteroTherapyServices.com

