CMS finalized new rules for Medicare Part B therapy services…and for once, some good news on issues that will directly impact therapy professionals!
CMS released the Physician Fee Schedule (PFS) Final Rule, a.k.a. the “Medicare Part B Rule,” outlining changes for 1/1/25. This 1,000+ page document includes information on payment rate changes, code changes, supervision of assistants, telehealth and more!
We highlighted the Medicare Part B rules that impact therapy in the SNF setting.
final Changes For January 1st, 2025
1. Rate Information
Rate cuts for Part B have been the norm in recent years, and 2025 will be no different. CMS is proposing a 2.93% decrease in the average payment rate under the Physician Fee Schedule (PFS) as compared to CY 2024, according to the CMS Fact Sheet.
Rate cuts are due to a 2.8% Conversion Factor (CF) decrease incorporating the expiration of the 2.93% “intervention” from Congress implemented in 2024, and a positive budget neutrality adjustment of 0.02%.
The new CF of $32.35 is a $.94 decrease from CY2024’s rate of $33.29, and has sadly been trending down for 6+ years.
The CF, a value that CMS modifies yearly, is part of the formula that determines the dollar amount for each CPT code by converting Relative Value Units (RVU). The CF impacts all Current Procedural Terminology (CPT) Codes across the board. When the CF decreases, the overall payment rate for the CPT codes decrease, unless the RVU for a specific CPT code is increased enough to offset the CF drop.
Did you know you can look up any CPT code and check the reimbursement rate HERE ? Knowing the reimbursement rates for each CPT code is valuable information for all therapy professionals!
2. Modifiers And Manual Medical Reviews
KX Modifier Threshold
The “old” Therapy Cap is now disguised as the KX Modifier Threshold, and “threshold amounts” change yearly. The 2024 “threshold” of $2,330 for OT, $2,330 for PT and Speech combined, will increase to $2,410 for CY2025. Continued use of the KX modifier is required for all therapy services that “would have exceeded the previous therapy cap amounts,” or claims will be automatically denied.
The KX Modifier is not simply a billing work-around. It’s an attestation by the therapist that the resident continues to require medically necessary services beyond the dollar threshold, and the rationale for the extended therapy services are documented in the medical record. All therapists should be aware of the amount of therapy a resident has received in a calendar year, and if over the threshold during a current episode of care, documentation should focus on supporting the extended services.
Manual Medical Review
The manual medical review threshold continues at the same amount of $3,000 until the next revision in CY2028.
This type of review is not automatic when the $3,000 is reached. CMS is uses the Targeted Probe and Educate (TPE) review process with providers identified through data submission as “outliers.” The TPE looks for providers with questionable practice patterns and provides training to decrease the error rate. For more information on the TPE process, visit the CMS info page or check out the Q&A Document.
3. Telehealth
As we are all well aware, therapy professionals were not able to provide telehealth services prior to the Public Health Emergency (PHE) and are only able to provide telehealth now post-PHE, through a temporary continuation of these extended flexibilities outlined in the Consolidated Appropriations Act through12/31/24.
The Final Rule confirms there are no active plans for an extension beyond the 12/31/24 expiration date from CMS.
On 12/31/24, telehealth under Medicare will end for therapy professionals. A change in law would be required to permanently add therapists to the approved telehealth provider list.
Additional Telehealth Rule Updates for 2025:
Telehealth will continue on in CY2025, even if therapy professionals are not added as approved providers. However, if there happens to be a miraculous extension for therapy professionals, this is important information to have. The Final Rule identified the following updates:
- Delivery requirements for Telehealth would allow the inclusion of two-way, real-time audio-only (vs the current requirement for audio-visual) communication technology for “any telehealth service furnished to a beneficiary in their home if”:
- The provider has the capability to provide 2-way audio-visual communications, though the inability to follow through is because of the patient. Meaning, “the patient is not capable of, or does not consent to, the use of video technology.”
- Modifier 93 must be appended to the claim for services described above to verify that these conditions have been met.
- Assuming the CPT code requirement can be met via audio-only
- The definition of Direct Supervision via telehealth to include audio-video communication “immediate availability” will be extended to 12/31/25, meaning “immediate availability” includes the use of audio/video, and need not be in person.
- 3 Care Giver Training codes were added to the provisional telehealth list:
- CPT code 97550, face-to-face with caregiver, without patient present
- CPT code 97551, face-to-face with caregiver, without patient present, each additional 15 minutes
- CPT code 97552, face-to-face with caregivers representing more than 1 patient, without patient present, Initial 30 minutes
CMS has not yet provided an updated list of Telehealth CPT Codes for CY2025. Below is the current list of acceptable codes:
Download CY 2024 List Of Telehealth Acceptable CPT Codes
4. Final changes to therapy-used cPT codes
Therapy Codes Getting Pay Increase
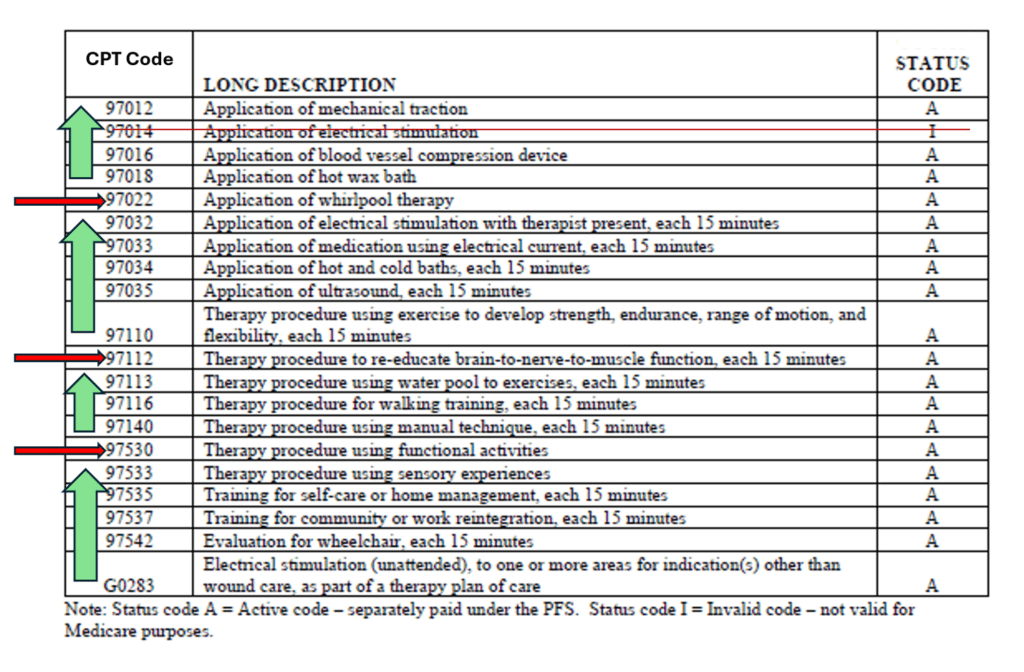
Professional Associations (APTA, AOTA) have been advocating for a review of “potentially misvalued codes” commonly used by therapy, to allow an increase in reimbursement. In the Final Rule, CMS agrees (finally) with updating the Practice Expense portion of the codes, which will change the reimbursement rates for the active codes below.
The results are an increase in 16 codes and decrease in 3 codes outlined below. Therapeutic Activities (97530), Neuromuscular Re-education (97112) and Whirlpool (97022) are the 3 codes proposed to have a reimbursement decrease, with all others showing an increase.
5. new rules for therapy practice
supervision of assistants redefined (pT & oT)
The long awaited regulatory change updating the Medicare definition of Supervision of Assistants finally made it to the Final Rule. Though this rule change speaks to the private practice setting and not the SNF, it is too good not to include here (and some SNFs also provide true outpatient therapy to the community and this will impact them as well).
CMS updated the current definition in the private practice setting from “direct supervision” to “general supervision,” to align with the definition in other practice settings. In the SNF setting, Medicare Part A and Part B have defined supervision as “general” for decades, and now it’s time for the private practice setting to join in. Assistants in private practice will no longer need the supervision of the therapist to be “on site,” and will transition to the therapist being “immediately accessible.” This change will be for all settings where therapists independently bill Medicare for their services (outpatient, mobile home care, etc.).
This Medicare requirement update is a “reimbursement rule,” and does not change State Practice Act requirements. The requirements of your State Practice Act may be more strict than Medicare’s definition change. If your State Practice Act for your particular therapy discipline requires on-site supervision, the Medicare rule is overridden. It’s possible that in some SNFs, PT, and OT will have different rules.
plan of care requirements redefined
The current requirements from Chapter 15 of the Medicare Benefit Policy Manual for physician certification of a Medicare Part B therapy “Plan of Care” (POC) require that the physician signs the Plan of Care within 30 days of the Initial Evaluation. If the POC is not signed timely, the certification requirement would not be met, which is a condition for billing. Treatment would need to stop until the certification is obtained.
What did the Final Rule Change?
In the Final Rule, CMS waived the requirement for physician signature on the Initial Plan of Care, as long as there is a physician order or referral for therapy services, and the order/referral is included in the medical record.
No physician order or referral for therapy services? Business as usual.
Having a copy of the referral or order for therapy in the record is the only way to avoid having to chase down the physician for a signature on the Initial POC.
- Send the Initial POC to the physician if you have an order/referral? Yes
- Need to obtain the physician signature? No
- Need proof that the POC was sent? Yes
- Send the Initial POC to the physician if you do no have an order/referral? Yes
- Need to obtain the physician signature? Yes
- Send all subsequent POCs AND obtain signature
In reality, the “new rule” is really only a “new exception to the rule” ….. an exception in needing the physician to sign the Initial Plan of Care Document” if there is an order/referral.
There are no changes to the Re-Certification Process. Send it, get it signed, track it.
Or better yet, just keep doing what you are doing!
In the SNF setting, best practice is to have a physician order for all residents, regardless of payor. Rules for each payor can differ, and going with the most stringent will save headaches (and win audits) going forward.
Important Links And Resources
Federal Register Copy (after 12/9/24)
In Summary
With every CMS Final Rule, we take the good with the bad. Some years it’s all bad. Not this year! Other than the rate cuts, the remaining rules impacting SNF therapy are positive for a change:
How would you label the following… Good or Bad?
- Rate cuts for CPT Codes will average 2.9%
- KX Modifier Threshold increased to $2,410 from $2,330
- Manual Medical Review Threshold remains $3,000
- Telehealth for therapy professionals will end 12/31/24
- Rates for 16 Commonly Used CPT Codes will increase
- Rates for 3 Commonly Used CPT Codes will decrease
- SNF General Supervision of Assistants will now be used in Private Practice
- Physician Signatures on the Part B Initial Therapy Plan of Care are no longer required if both of the following are in the medical record:
- An order (or referral) for therapy services
- Proof that the POC was sent to the physician
Remember, these changes are for Part B therapy only, and specific to the SNF setting. We teased out the parts of the Rule that applied to the SNF….so don’t worry about MIPS or other rules specific to private practice!
As always, if you have any questions about the information or how it will impact you, send them to us here: Just Ask Q&A
In Your Corner,
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
SNF Therapy & MDS Compliance Team
MonteroTherapyServices.com
REGISTRATION NOW OPEN
SNF REHAB MANAGER CERTIFICATION PROGRAM
STARTS FEBRUARY 12TH 2025 – SPACE LIMITED
