Centers for Medicare and Medicaid Services (CMS) released the Medicare Part A Skilled Nursing Facility (SNF) Prospective Payment System (PPS) FY2023 FINAL RULE containing the components that will go into effect 10/1/22.
The Final Rule contains the new Medicare Part A rates for the Patient Driven Payment Model (PDPM), new case mix index (CMI) values for each PDPM component, ICD-10 code mapping changes, and changes to the SNF Quality Reporting (SNF QRP) and SNF Value Based Purchasing (SNF VBP) programs.
Of particular interest to the SNF therapy and MDS professional, the final decision was made regarding the major topic in last year’s rule, “Recalibrating the PDPM Parity Adjustment.” [aka “How SNFs will pay back CMS $780 million] In last year’s Rule, CMS shared SNF coding and billing practice patterns that occurred during the first year of the PDPM that resulted in a 5% overpayment to SNFs, now requiring a necessary “recalibration.” The Final Rule sorts all of this out and how the “payback” will occur.
If you are interested in what the actual SNF therapy and MDS coding and billing issues were, this resource will help: CMS Release of PDPM Therapy Data
Below, the highlights for 10/1/22 that are most pertinent to SNF therapy and MDS professionals are reviewed.
Medicare Part A Payment Rate Changes
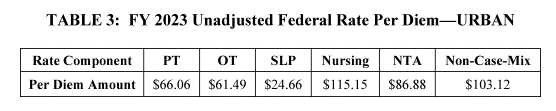
The Federal Per Diem rates are updated annually. On 10/1/22, the rates for Part A have a net increase of 2.7%, an increase of $904 million in payment to SNFs for FY2023, as compared to FY2022.
This net increase of 2.7% is the result after adding the Market Basket % increase of 3.9% + and the Forecast Error Correction of 1.5%, then subtracting the 0.3% Productivity Adjustment. What would be a 5.1% increase to Part A rates is then further reduced by 2.3% as part of the recalibration / payback noted above.
Of the options of how to repay the 4.6% parity adjustment, in the Final Rule, CMS opted for the phased-in approach of 2.3% Part A payment reduction per year over the next 2 years. The proposed amount was a 5% adjustment, which was then reduced to a 4.6% adjustment after CMS “parsed out the impact of COVID-19 PHE” on the data.
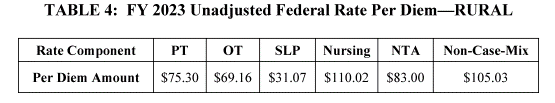
Below are the Final Unadjusted Rates for FY2023, that when multiplied by the case mix index values, determine each PDPM Case Mix Group rate….all showing an increase from last year.
What do these rate changes amount to for your SNF? A very basic example would be, if each of the 15,000 SNFs in the country split the $904 million equally, each would receive an additional $60,000 for the year. Obviously each SNF is unique in it’s Part A practice and the $904 million would be divided proportionately, though this gives a concrete example of what the rate increase looks like. It’s important to note here that this rate increase is before any reductions from the Value Based Purchasing Program and potential 2% penalty from the SNF Quality Reporting Program, discussed later.
So not a payment cut….but not a huge raise either!
Medicare Part A PDPM Changes – Case Mix Index Values
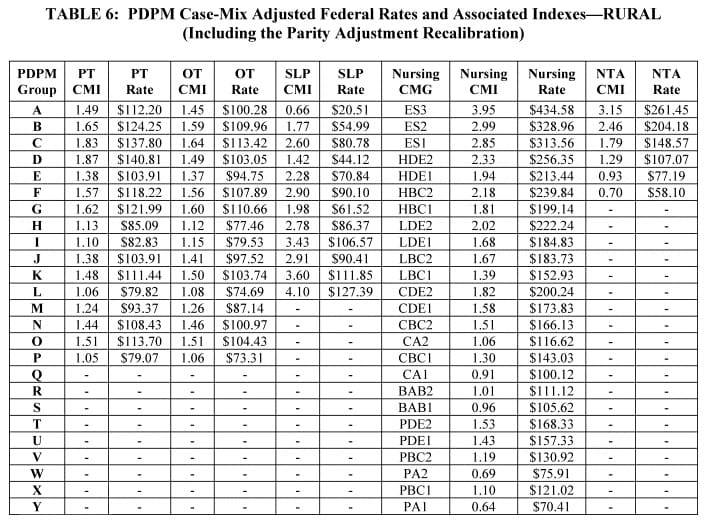
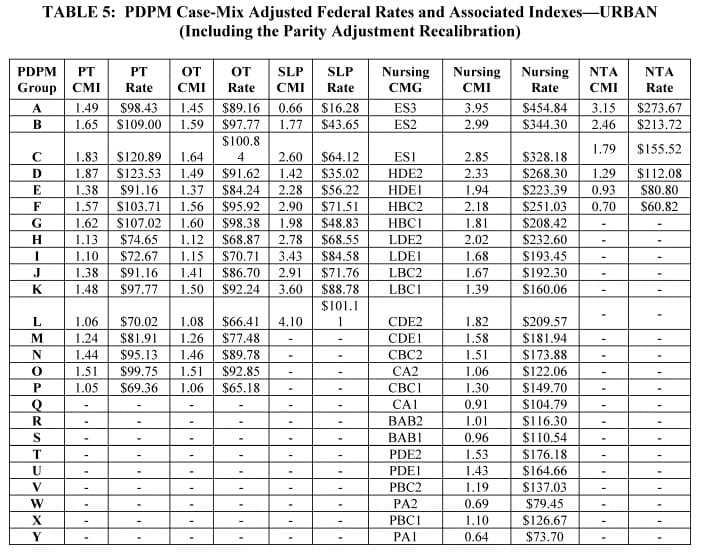
Case Mix Index (CMI) values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, have not changed over the past few years. However, for FY2023, CMI values for all PDPM components reflect the 2.3% decrease {payback}. When multiplied by the Unadjusted Federal Per Diem Rates shown above, rates for each case mix group will look like this on October 1st:
Changes In Wage Index – Geographical Locations – For Medicare Part A Calculation
Providers are deemed “urban” or “rural” for purposes of calculating the labor portion of the daily rate, a factor in determining the overall daily rate for a facility. Using wage index values specific to location to adjust the labor portion of the rate is done to reflect the wage differences throughout the country.
Simply stated…..reimbursement rates are different depending on where you live. The charts above are the Federal Rates. To get the exact rate for your SNF, the Wage Index for your location needs to be factored into the equation.
The updated Wage Index Tables for FY 2023 can be found below.
Not sure if you are urban or rural? Use the Wage Index Look Up Tool HERE
The FY 2023 SNF PPS final rule established a permanent 5% cap on annual wage index decreases to smooth the impact of year-to-year changes in SNF payments related to changes in the SNF wage index.
Medicare Part A PDPM Changes – ICD-10 Code Mapping for PT, OT and Speech Components
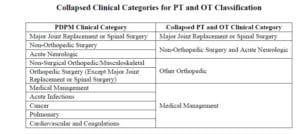
ICD-10 Codes used in MDS Section I0020B as the primary reason for SNF Part A covered care are used for case mix classification of the PT/OT Component under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, or identified as a Return to Provider code [meaning this code cannot be used in Section I0020B of the MDS].
Final ICD-10 Mapping changes for FY2023 are as follows:
- D75.839 “Thrombocytosis, unspecified,” currently mapped to “Cardiovascular and Coagulations” will be changed to “Return to Provider.”
- D89.44, “Hereditary alpha tryptasemia” currently mapped to “Medical Management” will be changed to “Return to Provider.”
- F32.A, “Depression, unspecified” currently mapped to “Medical Management” will be changed to “Return to Provider.”
- G92.9, “Unspecified toxic encephalopathy” currently mapped to “Acute Neurologic” will be changed to “Return to Provider.”
- M54.50, “Low back pain, unspecified” currently mapped to “Non-surgical Orthopedic/Musculoskeletal” will be change to “Return to Provider.”
- The following codes, now “Return to Provider,” will be mapped to “Medical Management:”
- K22.11, “Ulcer of esophagus with bleeding;”
- K25.0, “Acute gastric ulcer with hemorrhage;”
- K25.1, “Acute gastric ulcer with perforation;”
- K25.2, “Acute gastric ulcer with both hemorrhage and perforation;”
- K26.0, “Acute duodenal ulcer with hemorrhage;”
- K26.1, “Acute duodenal ulcer with perforation;”
- K26.2, “Acute duodenal ulcer with both hemorrhage and perforation;”
- K27.0 “Acute peptic ulcer, site unspecified with hemorrhage;”
- K27.1, “Acute peptic ulcer, site unspecified with perforation;”
- K27.2, “Acute peptic ulcer, site unspecified with both hemorrhage and perforation;”
- K28.0, “Acute gastrojejunal ulcer with hemorrhage;”
- K28.1, “Acute gastrojejunal ulcer with perforation;”
- K28.2, “Acute gastrojejunal ulcer with both hemorrhage and perforation;” and
- K29.01, “Acute gastritis with bleeding.”
CMS shot down provider requests to consider “Muscle Weakness” M62.81, as a mapped code, thus it will remain in the Return to Provider category due to it’s lack of specificity.
As of 10/1/22, the newly updated ICD-10 Mapping File will replace the current one. Here is the link:
FY 2023 PDPM ICD-10 Mapping (ZIP) (effective 10-01-2022)
Changes to CMS Medicare Part A Quality Programs
SNF Quality Reporting Program (SNF QRP)
The SNF QRP is the program behind Section GG, as well as other MDS data collection to measure multiple areas of care. This program has been around for over 6 years, and data collection for the multiple measures in this program will continue. Program cost to SNFs for FY2023 are estimated at $31 million.
This is a pay for reporting program, meaning, SNFs are required to report measure data, and if not reported, facilities will continue to be subject to a 2% Part A payment penalty. The penalty occurs for missing information, not for the data outcome. CMS wants your data!
What does missing data look like? MDS questions that have missing (dashed) data in select items. Here are the MDS questions for FY2023 that if dashed, categorize the MDS as having missing data.
Here are the 15 Measures in place for FY2023:
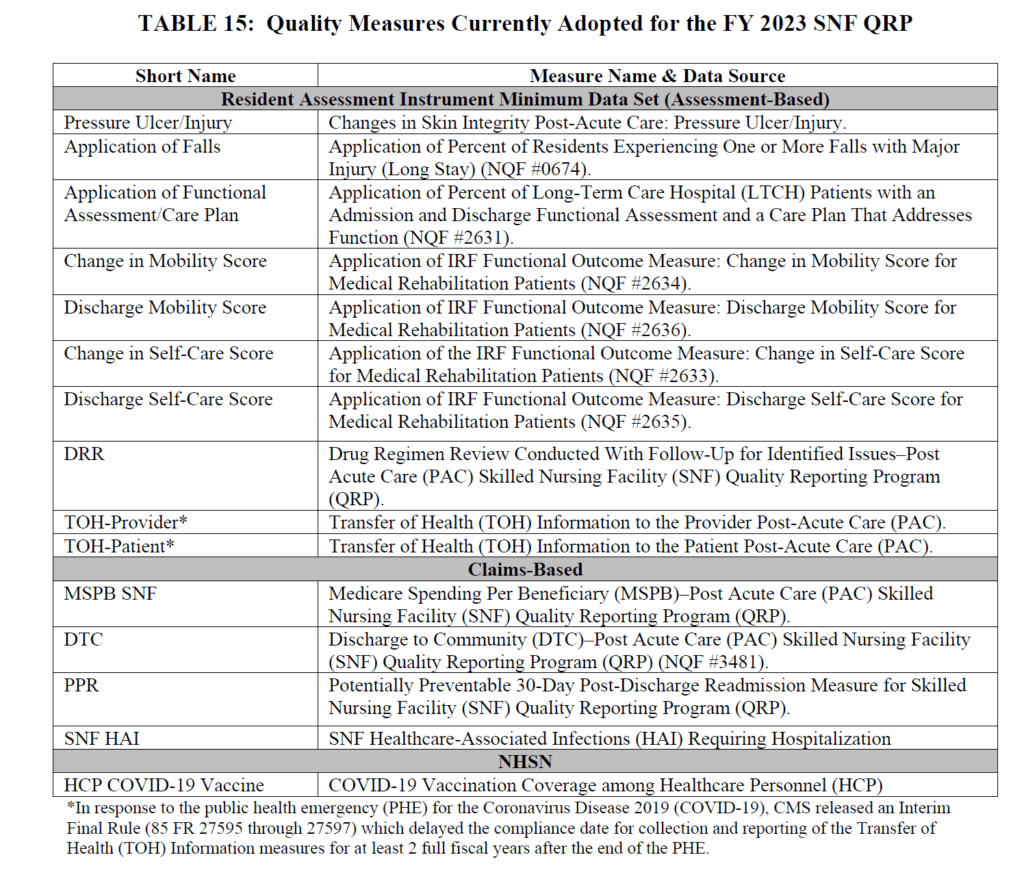
The last 2 measures above were discussed in detail in last year’s Final Rule and HERE, with a quick recap below:
- SNF Healthcare-Associated Infections Requiring Hospitalization measure (SNF HAI): This outcome measure collects data for infections acquired in the SNF resulting in re-hospitalization.
- COVID-19 Vaccination Coverage among Healthcare Personnel (HCP): This process measure tracks COVID-19 vaccination coverage among HCP in the SNF setting and publishes rates on Care Compare for the public
New SNF QRP Measures on the Horizon for 10/1/23 (FY2024):
- Influenza Vaccination Coverage Among Healthcare Personnel [NQF#0431]
- Data collection will begin 10/1/22 and end 3/31/23 (flu season) for 1st submission
- Submitted via CDC’s National Healthcare Safety Network (NHSN)
- Process measure of the % of HCP who receive the vaccine
- Denominator = # of HCP present in the facility for at least 1 day between 10/1-3/31
- Results will be publicly reported on Care Compare
- 2% Part A rate penalty for not reporting vaccination rates at 100% of required intervals
- Vaccination rates do not impact SNF reimbursement.
- Transfer of Health Information (Provider and Patient) Measures
- These 2 MDS measures above have been on hold while awaiting changes to the MDS and have now been released for a start next year
- Data collection will start 10/1/23 to coincide with the major MDS updates that kick in that day
- See the new MDS item set that includes the TOH questions in Section A HERE
- Standardized Patient Assessment Data Elements (SPADES)
- CMS adopted SPADES for the following categories collected on the MDS:
- Cognitive function and mental status
- Special services, treatments, and interventions (e.g., need for ventilator, dialysis, chemotherapy, and total parenteral nutrition)
- Medical conditions and comorbidities (e.g., diabetes, heart failure, and pressure ulcers)
- Impairments (e.g., incontinence; impaired ability to hear, see, or swallow)
- Data collection will start 10/1/23 on selected SPADES to coincide with the major MDS updates that kick in that day
- See the new MDS item set that includes the questions HERE
- Link to Measure information
- CMS adopted SPADES for the following categories collected on the MDS:
What do all these SNF QRP changes mean?
As the list of measures continues to grow, there is a greater chance of missing information and incurring a 2% payment penalty.
Starting 10/1/22, there are additional factors that may cause a 2% penalty if not monitored.
Not only do 80% of MDS assessments need to contain 100% of the SNF QRP required data in the designated MDS questions, now SNFs will also need to submit 100% of data for the COVID-19 AND Influenza Vaccination for Healthcare Personnel to the CDC NHSN system. 100%.
The full 2% penalty arises when either of the above requirements are not met, either on the MDS side, or the NHSN reporting side. And since the SNF QRP is always working the past and future simultaneously, the payment penalty for FY2023 stems from the data submitted [or not] in calendar year 2021.
- MDS data from CY2021 (At least 80% of MDSs with 100% of required data)
- COVID Vaccination reporting from Oct-Dec 2021 (100% of reported data)
The data being collected now will impact payment beginning 10/1/23. This includes the new Influenza Vaccine reporting requirement that kicks in this October 1st.
SNF Value-Based Purchasing Program (SNF VBP)
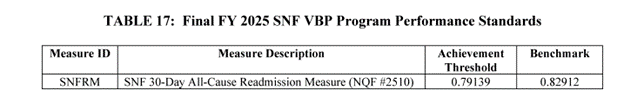
- The SNF VBP Program is the one that reduces Medicare Part A payments to all SNFs by 2% and then allows for an opportunity to recoup all or part of the 2% by demonstrating success with the established Quality Measure, SNF 30-Day-All-Cause Readmission Measure. In essence, this measures if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital. (“SNF Potentially Preventable Readmissions after Hospital Discharge Measure”)
- The Rule includes reductions in the VBP estimated at $186 million in payments to SNFs for FY2023.
- Continued suppression of the readmission measure data for scoring and payment purposes for FY2023 due to the PHE. This will include withholding the 2% required every year, followed by a 1.2% pay-back to SNFs (0.8% reduction for all). Plans to resume in FY2024.
- Continues to be publicly reported
- Achievement Threshold and Benchmark data for FY2025 as pictured here, though no significant changes were made to the program for FY2023 that will impact SNF therapy.
- Proposing to adopt 2 new measures for FY2026:
- SNF Healthcare Associated Infections Requiring Hospitalization
- Total Nursing Hours per Resident Day Staffing (Total Nurse Staffing) Measure
- Proposing 1 new measure for FY2027:
- Discharge to Community – Post Acute Care (Rate of successful discharge to community)
Other Areas Covered in the Rule
Changes to the requirements for Physical Environment/Life Safety Code and Director of Food and Nutrition can be found HERE.
In Summary
There is always a lot of information to digest for a successful October 1st transition each year. Thankfully the changes for this October will not bring about significant change in therapy or MDS practice. However, we are now on high alert for the major changes, particularly with the MDS, that will come about next October 1st.
Don’t forget to swap out your PDPM resources and new ICD-10 Mapping File on 10/1/22!
Additional Resources:
Link to the Final Rule and CMS Fact Sheet
PDPM Calculators and Resources will be updated with 10/1/22 data.
If you have any questions, send them to our Just Ask Q&A Forum and we will reach out to you to get your questions answered.
Thank you for all you are doing to provide the best care to the geriatric population!
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
Montero Therapy & MDS Compliance Resource