This comprehensive summary is intended to be a reference and teaching tool for SNF therapy and MDS professionals. With each passing year, the amount of information needed to digest grows and grows, and it can be overwhelming. Taking time to understand the information will help you help your facility succeed. Take it 1 bite at a time.
Part A Rate & PDPM Changes
SNF Quality Reporting Program (SNF QRP)
SNF Value Based Purchasing (SNF VBP)
Centers for Medicare and Medicaid Services (CMS) released the Medicare Part A Skilled Nursing Facility (SNF) Prospective Payment System (PPS) FY2025 Proposed Rule containing the components that will go into effect 10/1/24 pending any changes made based on comments submitted to CMS over the next few months.
The Proposed Rule provides updates to Part A rates, ICD-10 Code mapping for Patient Driven Payment Model (PDPM) calculations, SNF Quality Reporting Program (SNF QRP) changes, and SNF Value Based Purchasing (SNF VBP) updates. Let’s look at each of these areas.
Medicare Part A Rate & PDPM Changes
Medicare Part A Rates
The Federal Per Diem rates are updated annually. On 10/1/24, the rates for Part A have a proposed net increase of 4.1%, which means an increase of $1.3 billion in Medicare Part A payments to SNFs in FY2025. That may sound like a lot, but to put this in perspective, if all 15,000+ SNFs were created equal, this would equate to approximately $87,000 more per SNF. Individual SNF characteristics and track records with the SNF QRP and VBP impact the final outcome.
The details of how the 4.1% is derived can be found below.
- [(Market Basket increase of 2.8% + Forecast Error Correction of 1.7%) – 0.4% Productivity Adjustment (MFP)] = 4.1%.
- CMS updated one of the variables this year. The Market Basket base year was updated from 2018 to 2022. This type of update was last done 3 years ago when updating the base year from 2014 to 2018.
Below are the proposed Unadjusted Federal Per Diem rates used calculate each Patient Driven Payment Model (PDPM) Case Mix Group (CMG) rate.
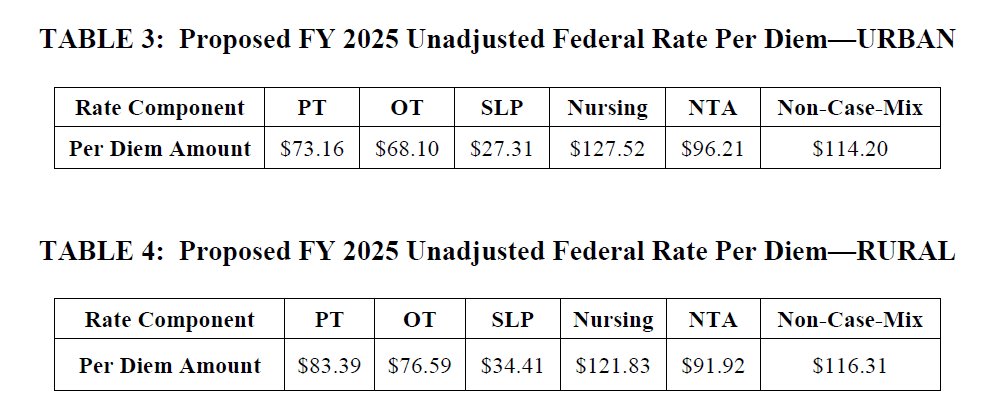
Now that we have daily per diem rate information, let’s put this together with changes to the Case Mix Index values in the next section to outline the individual rate for each Case Mix Group.
Medicare Part A PDPM Changes – Case Mix Index Values
Case Mix Index (CMI) values for each of the PDPM Components, PT, OT, Speech, Nursing and Non-Therapy Ancillary, are updated annually as needed. These values are important as they assign “weight” to each of the CMGs, and when multiplied by the daily per diem rates in the prior section, determine the rate for each individual CMG.
For the last 2 years, CMS reduced these values as a means to solve the problem of having SNFs “pay back CMS for overpayments” related to the “PDPM Recalibration.” CMS adjusted the CMI values to produce an overall lower Medicare Part A daily payment rate. Thankfully, we are over the recalibration hurdle now, and the CMI values for each of the 5 components for 10/1/24 will be the same as last year. The dollar values will be different, of course, due to the rate changes, but the CMI values will remain the same.
Here are the proposed “adjusted” daily rates for each of the case mix groups (CMG), derived by multiplying the Unadjusted Federal Per Diem Rate with the CMI value assigned to each CMG. These are the pieces needed in order to calculate the total daily rate.
Total Daily Rate = PT + OT + SLP + Nursing + NTA + Non-Case Mix Rate
Proposed FY2025 (Urban)
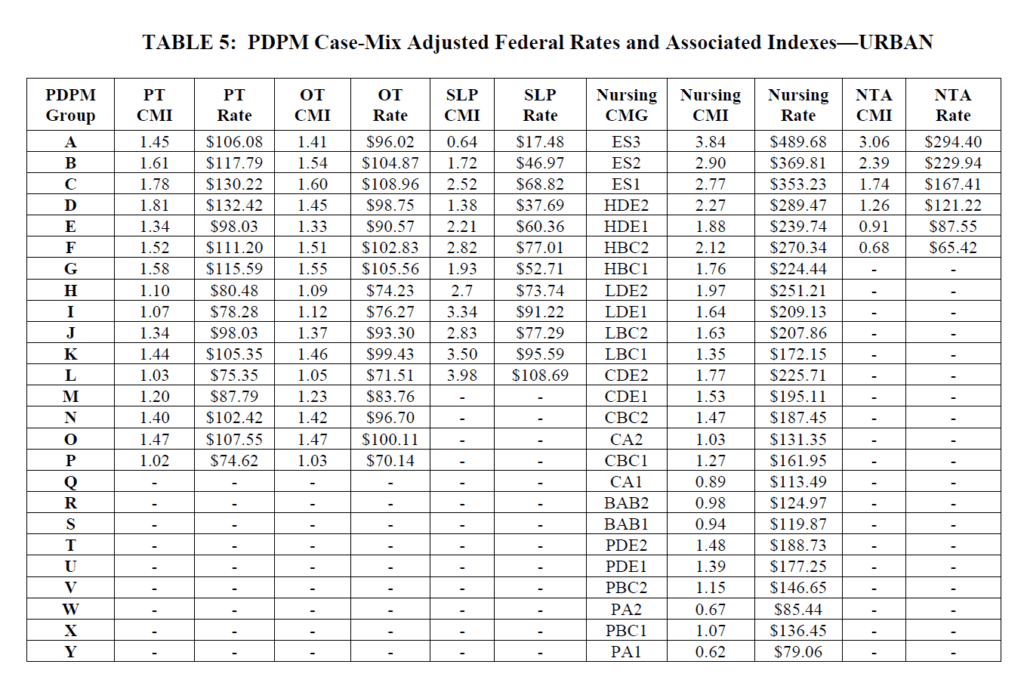
As a reminder, all of the CMG scores come from the MDS and how trigger questions are answered. The Non-Case Mix Group Rate is a “flat rate,” not tied to the MDS.
For example, using the chart above, a HIPPS Code of KACD1 represents TK [PT $105.35] + TK [OT $99.43] + SA [SLP $17.48] + ES1 [Nursing $353.23] + ND [NTA$121.22] + Non-Case Mix Rate [$114.20]. The total base rate for this HIPPS Code would be $810.91 per day.
The total base rate per day fluctuates based on what “PPS day” it is. Days 1-3 see a higher rate due to the NTA Component paying triple, and days 21-100 see a rate reduction as the PT and OT Component slowly decreases in value throughout the stay.
Changes In Wage Index – Geographical Locations – For part a rate calculation
In the section above, we demonstrated how to calculate the daily per diem rate. To take this rate and transform it into the rate that your SNF will receive, requires another piece of the puzzle…. the Wage Index (WI).
CMS categorizes SNFs as Urban or Rural and assigns a unique WI value to each county or state. This WI is a variable used to take the Total Daily Per Diem Rate and adjust it up or down based on where you live.
The total daily rate explained in the section above is comprised of a Labor Portion and a Non-Labor Portion. The WI is used to adjust the Labor Portion to get your location-specific rate.
Total Daily Rate = Labor Portion + Non-Labor Portion
Your SNFs Total Daily Rate = (Labor Portion x Your SNFs Wage Index) + Non-Labor Portion
CMS updates these WI values each year. The proposed Wage Index Tables for FY 2025 can be found here:
The Proposed Rule makes some changes to the Urban and Rural classification, flipping 54 counties from Urban to Rural, and 54 more from Rural to Urban. The Rule also changes the way some of the counties are grouped together, impacting the overall rate for many.
Make note of whether your SNF is Urban or Rural, and your area WI. Not sure if your SNF is classified as urban or rural? Use the Wage Index Look Up Tool HERE and plug that into the PDPM Calculator to get your rates.
Medicare Part A PDPM Changes: ICD-10 Code Mapping For PT, OT And Speech Components
The ICD-10 Code selected for MDS Section I0020B as the primary reason for SNF Part A covered care is used for case mix classification under PDPM. Using the Mapping Tool provided by CMS, each ICD-10 Code can be mapped to 1 of 4 PT and OT Clinical Categories as shown here, or identified as a Return to Provider code.
In other words, Return to Provider Codes can’t be used to represent the primary reason for skilled care in Section I0020B, and the code that is used in this Section will fall into 1 of the 4 collapsed Clinical Categories below, thus, determining the PT/OT Component grouping.
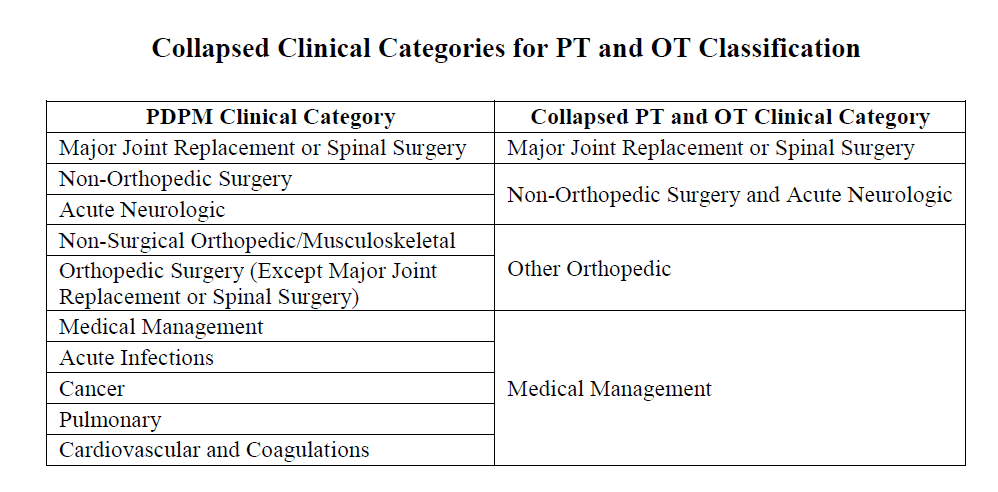
Each year, CMS makes modifications to the mapping of certain ICD-10 Codes. Believe it or not, there are only 4 code changes for FY2025, proposed to change the mapping from Medical Management to Return to Provider.
Medical Management to Return to Provider
- E88.10 Metabolic Syndrome
- E88.811 Insulin Resistance Syndrome, Type A
- E88.818 Other Insulin Resistance
- E88.819 Insulin Resistance, Unspecified
CMS typically releases the official DRAFT ICD-10 Mapping File with the rule, though this is yet to come. With only 4 changes to this section, there’s no rush.
Changes to the Non-Therapy Ancillary (NTA) Component
Potential changes to the NTA Component are the highlight of the Rule. According to CMS, the NTA Component will change, but not on 10/1/24. The “future” changes to this component are “under consideration” but need our attention now.
The intention in the Proposed Rule is to solicit information about potential future changes, and CMS has laid out for us what those changes may be. It seems like CMS has put quite a bit of effort into changes that “may or may not happen” in the future.
See what you think…..
In the Proposed Rule, CMS has a Request for Information (RFI) for updates to the NTA Component. Now that CMS has a few years of actual NTA and Part A PDPM claims data, the goal is to use this (FY2019-2022) information to make some updates. Proposed updates also include modifying where the NTA points “come from.” We know that points can come either from checkboxes on the MDS or by adding ICD-10 Codes to Section I8000 from the Mapping Files, and there can often be confusion, as some point categories are listed in both places, but the points can only come from one source. CMS proposes to rely more on MDS checkboxes when possible.
A NTA Component simplification process for coding will be welcomed! Our chart reviews often identify missed NTA point opportunity simply based on the inconsistencies of the component. Here are a few current examples that illustrate why clarification in the NTA Component would be welcomed:
- Checking Cirrhosis in Section I1100 will not capture 1 NTA point. The ICD-10 code from the CMS Mapping File under the Cirrhosis category must be entered into Section I8000 for the point.
- Checking Respiratory Failure in Section I6300 will not capture 1 NTA point. The corresponding ICD-10 Code from the CMS Mapping File under Cardio-Respiratory Failure and Shock is required to gain the point.
Eliminating the duplication will improve accurate coding and reimbursement.
Potential Changes to the NTA Component Point Value
Do you want the good news or the bad news first?
The changes under consideration to the NTA Component are shown below. This is what the “new NTA Point List” would look like if all changes were made.
Points highlighted in red reflect a reduction from the current point value, and green, an increase in point value.
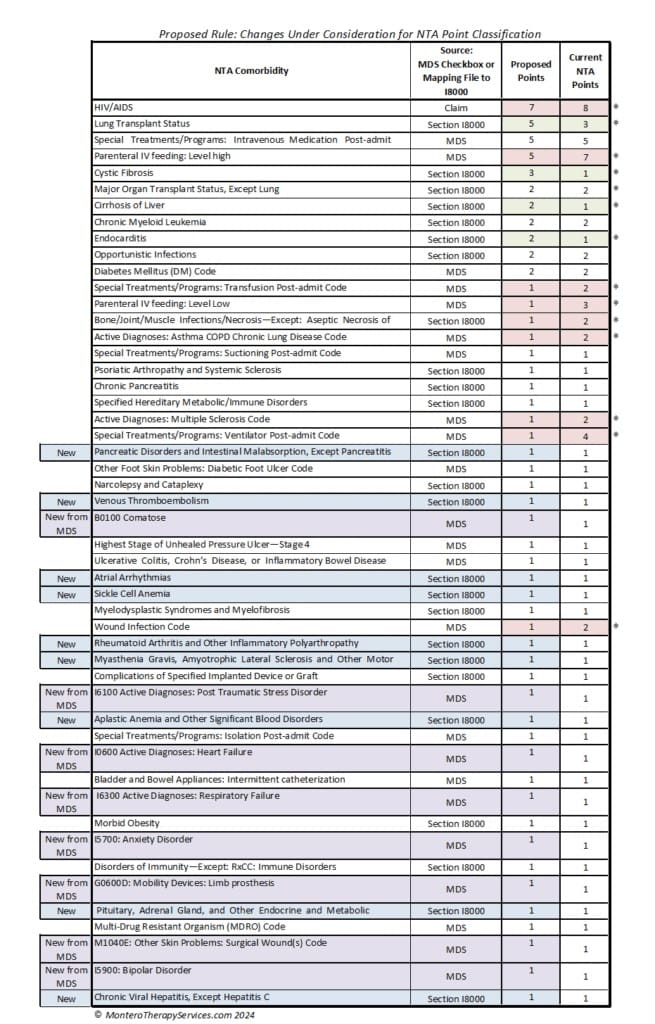
Dropping in point value are: HIV/AIDS, IV Feeding: High and Low Level, Transfusion Post Admit, Bone/Joint/Muscle Infections, I6200 Asthma/COPD, Ventilator Post Admit, Multiple Sclerosis, and Wound Infection.
Gaining point value are: Lung Transplant Status, Cystic Fibrosis, Cirrhosis, and Endocarditis.
The blue and purple areas represent the additions to the NTA point family. These include MDS checkbox items and Section I8000 add-ons. It is interesting to see some of these checkbox additions:
- Section B: Comatose
- Section G: Limb Prosthesis
- Section I: PTSD, Heart Failure, Respiratory Failure, Anxiety Disorder, and Bipolar Disorder
- Section M: Surgical Wounds
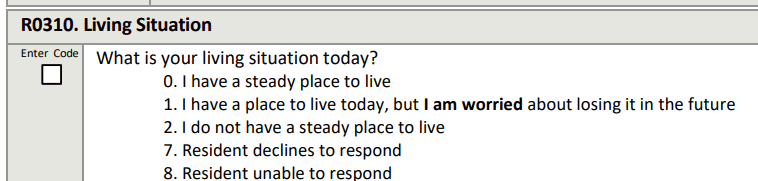
NTA Point Categories Removed From The List
Last but not least, let’s look at NTA points that would be leaving us. Though the categories for removal only have 1 point value, we know that only 1 point is needed to move from NF to NE… a big difference in reimbursement!
There are some frequent flyers here that will make a big difference in facility comorbidity scores if removed. It’s not a shocker to see Malnutrition, among others, on the list.
If you are going to send comments to CMS about anything…. this is it.
The original CMS NTA Fact Sheet states that “classification is determined by the presence of certain conditions or the use of certain extensive services that were found to be correlated with increases in NTA costs for SNF patients.“
When looking at the list of NTA points being removed, the question becomes “what about the increased costs associated with them?” Some of these items are not even represented for reimbursement in any of the other PDPM Components (ie: Nursing Component). How will they be reimbursed? (Ostomy supplies, Malnutrition supplements…)
Insert Deep Breath Here….
Changes To CMS Medicare Part A Quality Measure Programs
If you are not already heavily involved in your SNF Quality Measure Program processes, NOW is the time. As these Measure Programs grow and grow, don’t get left behind. By understanding the Measures and Programs, SNF therapy and MDS professionals can be a godsend to their facility. Here, we break down each program and what will be changing.
SNF Quality Reporting Program – SNF QRP
The SNF QRP is the program that started small over 8 years ago [remember when Section GG was new?] and is now ballooning into the program with the most measures. This is a pay for reporting program, meaning, SNFs are required to report measure data, and if not reported, facilities will be subject to a 2% Part A payment penalty.
The penalty occurs when information is missing, not for poor outcomes. [yet]
What does missing data look like? MDS questions that have (dashed) data in select items, or information that is required to be provided directly from the SNF to the CDC’s National Healthcare Safety Network (NHSN), both count toward “missing data.”
Here is a link to all the MDS questions that, if not filled out, will trigger the payment penalty if the threshold is met.
For the present CY2024 collection period, both the current MDS and the MDS with updates due 10/1/24 are in play. The list of item sets (MDS questions) continues to grow, making the attainment of submitting100% data on 90% of all Part A MDSs a challenge.
Make sure MDS staff have the list of MDS items above. These are the MDS items being collected NOW that will potentially impact FY 2026 Annual Payment Update (APU) Determination.
Don’t lose 2%!!
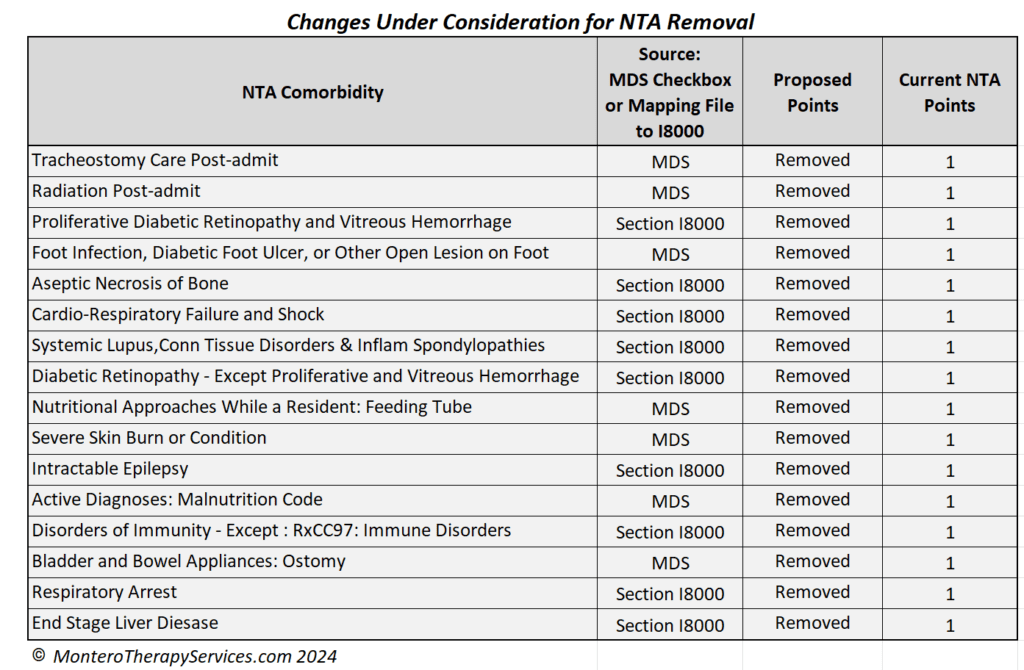
Here are the 15 Measures in place for FY2025
The list is a little shorter this year due to the removal of 3 Measures that involved Section GG:
- Admission and Discharge Functional Assessment /Care Plan That Addresses Function – Requiring 1 Discharge Goal
- Change in Self-Care Score
- Change in Mobility Score
But don’t worry, the Measures that were approved in the prior year are now on the list:
- Discharge Function Score Measure
- Outcome measure from Section GG Self Care and Mobility Technical Report
- Calculated % of Part A residents who meet or exceed DC Function Score
- Uses 10 GG items: Eating, Oral Hygiene, Toileting Hygiene, Roll L/R, Lying to Sit, Sit to Stand, Transfer, Toilet Transfer, Walking 10′ and Walking/Wheeling 50′
- Data collection started 10/1/2023
- COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) Measure
- Report the number of HCP who are up to date with recommended COVID-19 vaccinations
- Data collection started 10/1/23
- COVID-19 Vaccine: Percent of Residents Who Are Up to Date
- Data collection starts 10/1/24 with the addition of new MDS question to capture the data
Newly Proposed measures….
CMS is not proposing to adopt any “new” Measures in the Rule. However, there are some changes to be aware of with “existing” measures, including new MDS data elements (questions).
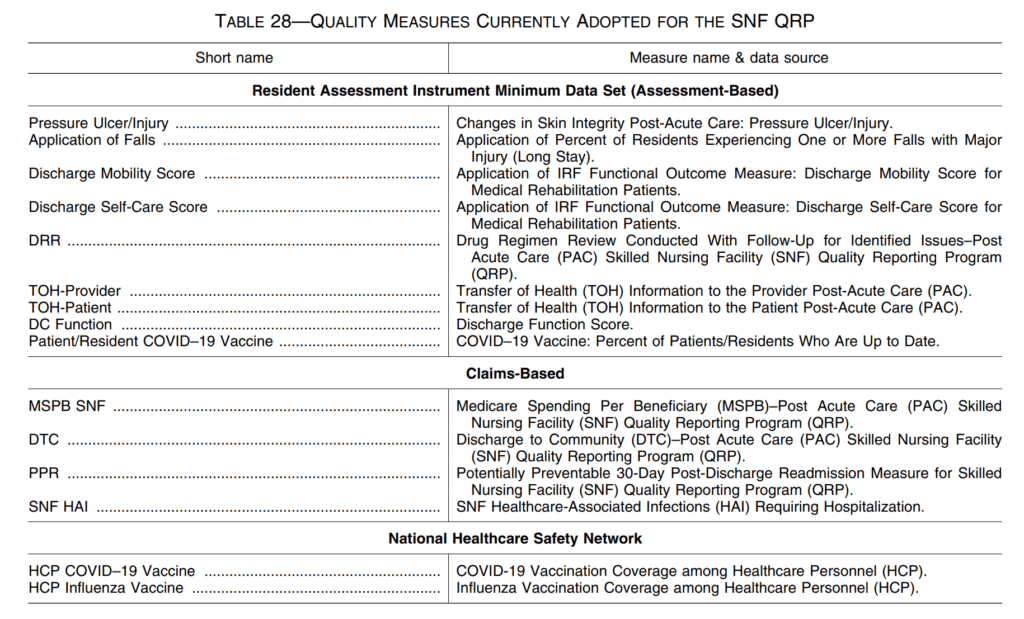
CMS is proposing to add 4 new items as Standardized Patient Assessment Data Elements (SPADES) under the Social Determinants of Health (SDOH) category, and modifying 1 existing element.
SDOH are defined as the socioeconomic, cultural, and environmental circumstances in which individuals live that impact their health. SPADES are the data elements (MDS item questions) that are standardized across all post acute care settings (ie: Home care, Inpatient Rehab, SNF). For example, this is why we see GG Items collected in multiple settings.
Data collection for these items would be for new admissions only beginning 10/1/25 through 12/31/25, once these items are added to the MDS, with a payment impact in FY2027. Starting in 2026, data collection would shift to a calendar year (CY), with CY 2026 data impacting payment for FY2028.
The 4 New MDS Questions on medicare pPS 5-day
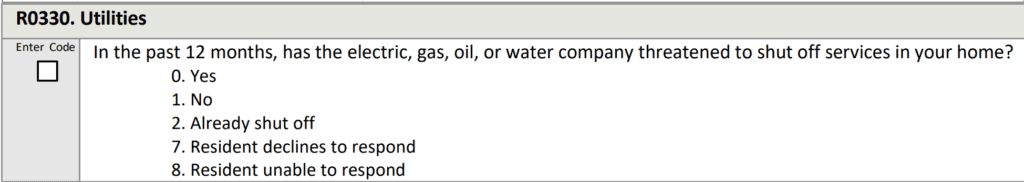
Below are the 4 new items, each proposed to collect information on admission, that will allow the SNF to collaborate with additional agencies for support of the resident upon discharge.
Living Situation:
Food (x2):
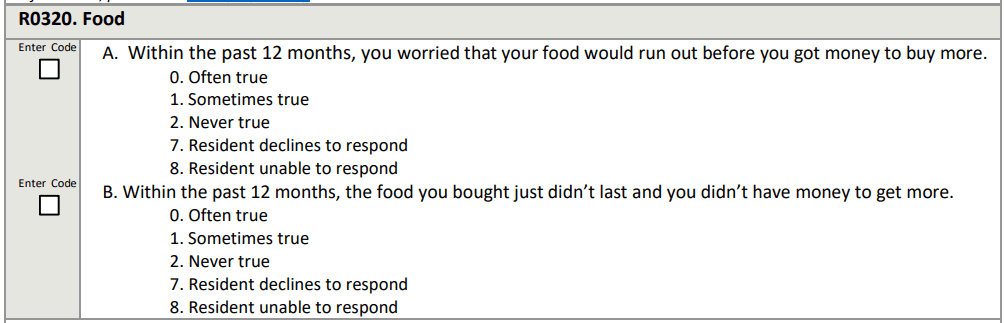
Utilities:
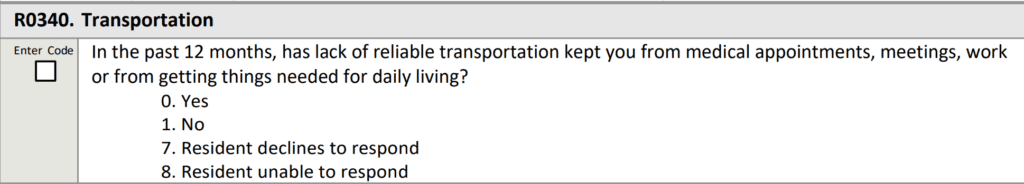
1 Modified MDS Question on Medicare PPS 5-day
CMS is proposing a modification of the existing Transportation Item in Section A1250 to clarify a look-back window and simplify the response options. This item is proposed for FY2027 for new admissions only, no longer requiring completion at discharge, and will move from Section A of the MDS to a new “Section R.”
Greater Chance for 2% Payment Penalty
As of 1/1/2024, the required MDS data reporting threshold increased from 80% to 90%, with a payment impact beginning 10/1/25. This means CMS requires SNFs to report 100 percent of the required quality measures data and standardized patient assessment data collected on at least 90 percent of all PPS Part A assessments submitted beginning with the FY 2026 SNF QRP.
The SNF QRP works in 2 time tables. The collection of data NOW [reporting period] will impact your payment in the FUTURE.
As the list of measures continues to grow, there is a greater chance of missing information and incurring a 2% payment penalty. Not only do 90% of MDS assessments need to contain 100% of the SNF QRP required data from the MDS, SNFs also need to submit 100% of data for the COVID-19 and Influenza Vaccination for Healthcare Personnel to the CDC NHSN system. If info is missing either way, the penalty will apply. This does not leave much room for error.
Future Validation Process of SNF QRP Measures
SNF QRP Measures require validation and CMS is proposing methods to validate both the MDS and Part A claims data beginning FY2027. The Proposed Rule outlines a process using a validation contractor that will request up to 10 records per year from 1,500 SNFs, aligning the QRP record review with the VBP review so the same residents are used for selection.
Records from CY2024 [NOW!] would be selected for the FY 2027 validation process. Failure to submit records will result in a future (2 years out) 2% payment penalty.
The Rule also mentions the possibility of including a MDS validation review process in the future to determine if what is coded on the MDS is supported in the record, potentially challenging PDPM reimbursement items (….like the 5-Record TPE Audits all SNFs had…only expanded ….and permanent).
Future SNF QRP Measures
In the Proposed Rule, CMS is seeking comments (RFI) on 4 potential future areas of the SNF QRP. CMS states they intend to use this input to inform future measure development efforts.
These areas of interest include:
- Overall immunization status
- Pain Management
- Depression
- Patient Satisfaction
On to the last quality measure Program….
SNF Value-Based Purchasing Program (SNF VBP)
The SNF VPB Program works by reducing Medicare Part A payments to ALL SNFs by 2% and then allows for an opportunity to recoup part of the 2% by demonstrating success with the established Measure. These “incentive payments” are intended to encourage SNF improvements in the quality of care provided to Medicare beneficiaries.
Since the start of this Program, there has only been 1 Measure: The SNF 30-Day-All-Cause Readmission Measure, which looks at if the resident was readmitted back to the hospital within 30 days of being discharged from the hospital to the SNF.
Though there are no new measures in this year’s Proposed Rule, we are all impacted by the multitude of new measures added over the past 2 years that are now kicking in.
In addition to the only Measure currently in play (SNFRM), this is the full list of adopted Measures. Performance period data collection began on 10/1/23 for Measures 2-5 on the list below. The Program Year is typically 2 years after the Performance Year, so attention needs to be paid to the Performance Year when the actual data is collected.
When the Program Year hits, it’s too late to do anything about the data.
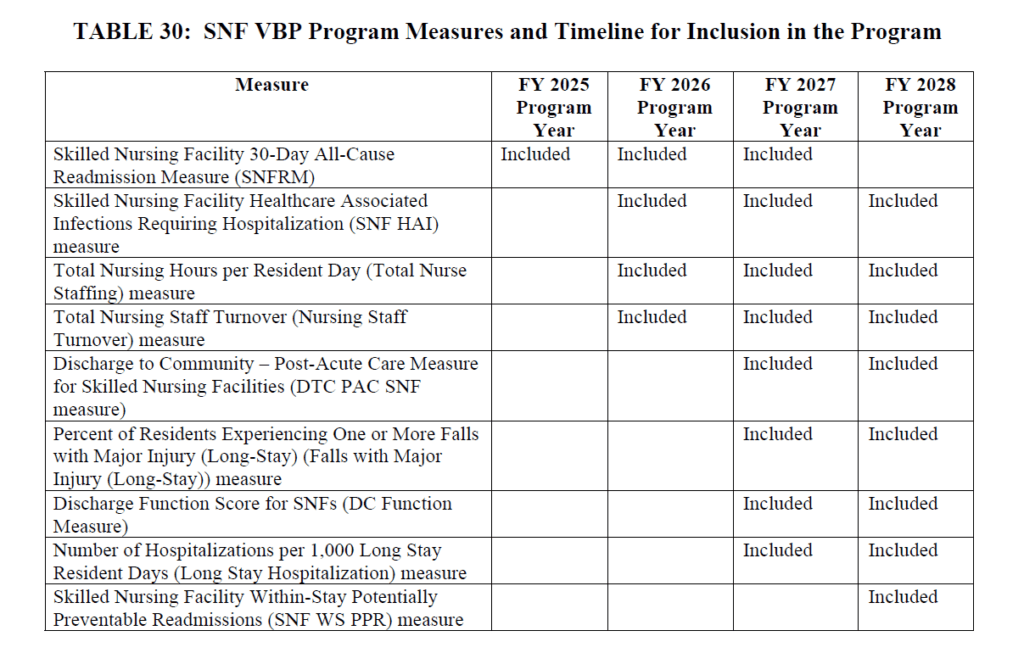
The last 4 Measures on the list above are waiting on deck with data collection to start 10/1/24.
- Falls with Major Injury (MDS Measure includes long-stay residents)
- Already a QM in other programs, used in 5 Star and publicly reported
- Data collection starts 10/1/24 with payment impact 10/1/26
- Discharge Function Score (MDS Measure)
- Same Measure from SNF QRP
- Uses 10 Section GG items: Eating, Oral Hygiene, Toileting Hygiene, Roll L/R, Lying to Sit, Sit to Stand, Transfer, Toilet Transfer, Walk 10′ and Walk 50′/Wheel 50′
- Data collection starts 10/1/24, impacts payment 10/1/26
- # of Hospitalizations per 1,000 Long Stay Resident Days (Claims Measure)
- Already publicly reported and used for 5 Star
- Data collection starts 10/1/24
- SNF With-Stay Potentially Preventable Readmission Measure (FY2028) (Claims Measure)
- Replaces the SNFRM with a modification of the previously proposed “SNF Potentially Preventable Readmission After Hospital DC Measure.”
- Data collection FY2025 and 2026 for payment impact FY2028
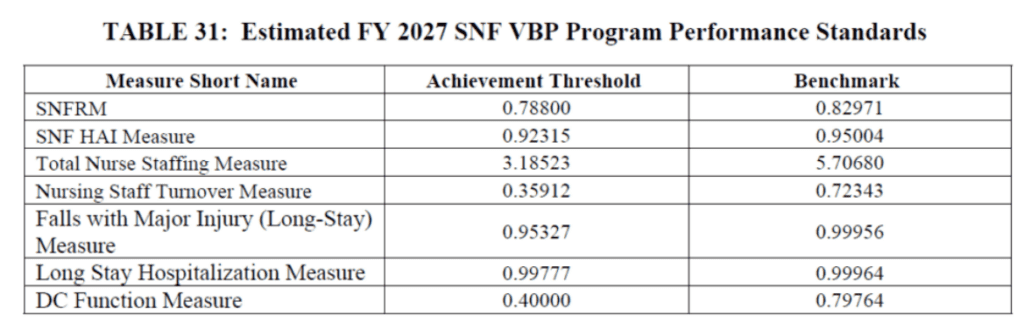
SNF VBP Measure Performance Standards
The Proposed Rule released the Achievement Threshold and Benchmark for each of the VBP Measures as shown below.
Are we done yet???
Though we will not go into the details here, it is important to know that the Proposed Rule has a full section dedicated to Nursing Home Enforcement, outlining “the Biden-Harris Administration commitment to ensuring that all residents living in nursing homes receive safe, high-quality care.” The proposed rules give CMS greater flexibility by removing some restrictions on how rules are enforced, Civil Monetary Penalties for health and safety violations, etc. This portion of the Proposed Rule has created quite a stir and will be addressed separately.
What’s Next?
CMS is accepting comments for the proposed rule through May 28, 2024.
We know from past results that comments submitted have the potential to influence CMS decisions. Consider commenting on an area you are passionate about. You never know!
Electronic comments can be made at https://www.regulations.gov Follow the “Submit a comment” instructions.
Additional Resources:
HERE is a link to the Proposed Rule. PDF Version
HERE is a link to the CMS Fact Sheet.
PDPM Calculators and Resources HERE
If you have any questions, send them to our Just Ask Q&A Forum and we will get your questions answered.
Thank you for all you are doing to provide the best care to the geriatric population!
In your corner,
Dolores
Dolores Montero, PT, DPT, RAC-CT, RAC-CTA
President | Montero Therapy & MDS Resource Team
MonteroTherapyServices.com
next rehab manager certification course starts july 10th
If you would would like an email when registration opens, leave your information here.
